Gastric Bypass Surgery: Yesterday and Today
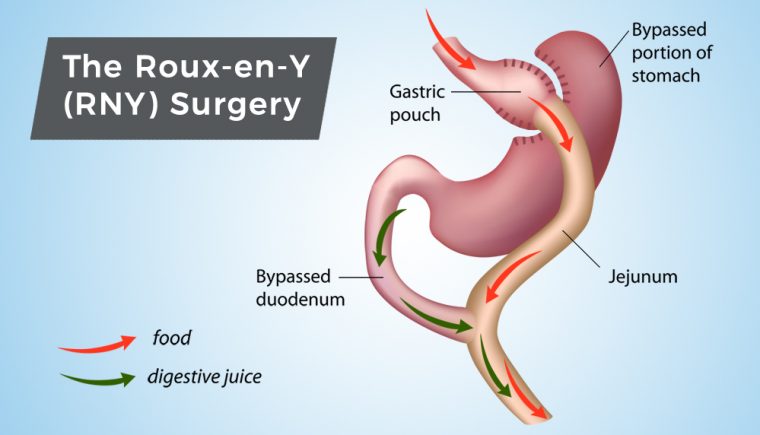
May 31, 2017Obesity is a serious disease affecting millions of people worldwide and the percentages continue to increase. This is significant since obesity is associated with other medical problems that negatively impact patients’ quality-of-life and risk of death (heart disease, for example). Given this trend, obesity treatment has been likewise increasing. I would like to discuss the role of Roux-en-Y Gastric Bypass in the treatment of morbid obesity, and how the procedure has improved from past years to today.
Gastric Bypass RNY: Yesterday
The first Gastric Bypass surgery was initially performed in 1966 using one large incision (open surgery). The open operation is associated with greater risk of complications. This ultimately led to the performance of the first Laparoscopic Roux-en-Y Gastric Bypass in 1994 (4-6 tiny incisions). Over time, the laparoscopic approach has been shown to be performed with fewer complications, leading to a switch from the open approach to the laparoscopic surgery in 2004-2005.
When the Gastric Bypass was originally performed, the risks for serious complications and mortality were higher than they are currently. The risk of dying after surgery was reported to be 1 in 100 (1%) early in the mid-2000’s. With currently performed Laparoscopic Roux-en-Y Gastric Bypass surgery the mortality rate is less than 3 in 1000 (0.3%) patients, which is lower than most major abdominal operations.
Gastric Bypass RNY: Today
 The Gastric Bypass of “today” is certainly not the Gastric Bypass of “yesterday.” As the field of weight loss surgery continues to grow, our knowledge about these procedures increases with continued improvements in safety and success. The Gastric Bypass of “yesterday” is associated with a higher rate complications, longer hospital stay (2-4 days), increased chances of having an open (big incision) operation and lower long-term survival rates. “Today” the Gastric Bypass is associated with a shorter hospital stay (1-2 days), a greater chance of having a laparoscopic procedure, improved cosmesis, fewer complications, improved quality of life and an increase in long-term survival rates.
The Gastric Bypass of “today” is certainly not the Gastric Bypass of “yesterday.” As the field of weight loss surgery continues to grow, our knowledge about these procedures increases with continued improvements in safety and success. The Gastric Bypass of “yesterday” is associated with a higher rate complications, longer hospital stay (2-4 days), increased chances of having an open (big incision) operation and lower long-term survival rates. “Today” the Gastric Bypass is associated with a shorter hospital stay (1-2 days), a greater chance of having a laparoscopic procedure, improved cosmesis, fewer complications, improved quality of life and an increase in long-term survival rates.
Another important distinction between “yesterday” and “today”, with regards to Gastric Bypass surgery, is the counseling process. Many patients “yesterday” underwent operations without preoperative counseling and were discharged without the proper education about their operation. This resulted in less optimal outcomes because the patient did not know what to expect, how to use their tool afterward or the signs/symptoms of complications.
Currently, all accredited programs provide excellent education before and after surgery, thereby improving the patients’ understanding of the process, how to optimally use their tool, and how to monitor for complication that should be managed by a bariatric surgeon.
When I counsel patients regarding bariatric surgical operations, patients often state that they do not want to have that "dangerous Gastric Bypass operation." However, the Gastric Bypass may be the best option for some patients, such as those patients with severe heartburn or reflux symptoms, more advanced diabetes mellitus type 2 and higher BMI.
Several studies have been performed in recent years demonstrating an overall decrease in dying from all causes for patients undergoing Laparoscopic Roux-en-Y Gastric Bypass. When considering this, patients are at greater risk of death from obesity, and its associated medical problems, than from Gastric Bypass surgery.
Another reason one would consider surgery is the significant improvement in medical co-morbidities and decrease in medication use.
- Greater than 80% of patients will stop taking all of their diabetes medications postoperatively
- Approximately 45% of patients will stop taking high blood pressure and cholesterol medication
- Weight loss is also excellent, with the majority of patients achieving a weight loss of 70% of their excess weight (33% of their total body weight).
I have seen patients who had surgery for a complication after Gastric Bypass and someone says: “Mrs. X had that obesity operation and now look what happened.” Every day in this country people undergo operations for other medical issues, that are arguably less severe than morbid obesity. However, for some reason, complications of these procedures are accepted. I don’t quite comprehend why it is perceived as reasonable for a patient who smokes and has a complication after surgery to remove cancer to accept complications as an understandable part of having a big operation?
"When it comes to obesity, and apparently, the prejudice surrounding it, postoperative complications are a tragedy from having an “unnecessary” operation. As a bariatric surgeon, I find this perception detrimental to the care of bariatric patients." ~ Dr. Tracy Pitt
In conclusion, a laparoscopic Gastric Bypass can be safely performed for patients with excess weight with excellent overall outcomes.
 | ABOUT THE AUTHOR Dr. Tracy Pitt is a board-certified general surgeon at JourneyLite of Cincinnati who is fellowship trained in minimally invasive surgery and specializes in weight loss surgery. Dr. Pitt is a native of Northeast Ohio and completed his General surgery residency at South Pointe Hospital in Cleveland, Ohio. He subsequently completed fellowship training in Advanced Laparoscopic and Bariatric surgery at the Cleveland Clinic in Cleveland, Ohio. |



