FemmeMode
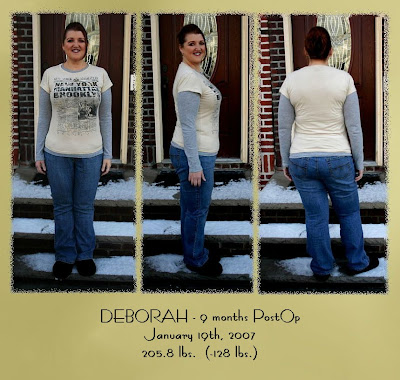
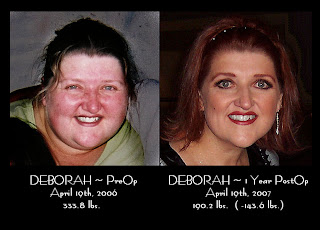
One Year SURGIVERSARY Pictures...
Apr 19, 2007
 WOW....
WOW.... 
(CLICK on the photos for larger view...)
ONE YEAR Surgiversary!!
Apr 19, 2007
Saturday, August 13, 2005
Wake-Up..."Wake-Up Call...."
I’m ready to go and get the information to get started with weight loss surgery. Today was my daughters 2nd birthday…there are SO many things I currently hold back, or miss out on. Her god-mother was sooo fun with her today at Chuck E. Cheese’s….
In the play arena at Chuck E. Cheese’s they have a huge crawl tube attached to the ceiling….the kiddos climb up these obstacle ladders…and then crawl thru these tubes that maze thru on the ceiling. I would NEVER be able to let her enjoy that…thankfully her godmother is soooo fun and adventurous! It rang home in a pain to my heart how my weight can subtly affect my two-year-old RIGHT NOW!! I don’t like to take her to the park – for fear if she runs too far from me I won’t be able to run after her. No more – I’m calling MONDAY!!!
____________________________________________________________
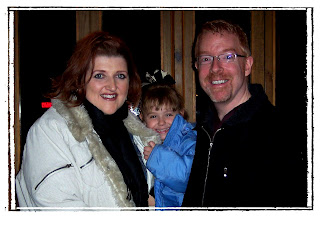
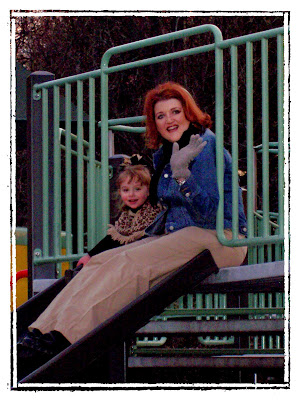 I remembered this blog when I was looking thru the pictures we took today on my Surgiversary. My sweet Husband came home from school in the afternoon today....and we first took Isabella to the park together...and then all went out to dinner!When we got home...I saw russ had taken a BUNCH of pictures of Isabella and I playing 'tag/chase' on the jungle gym playground....These pictures are soooo precious to me....they are not very good quality....but I love them!
I remembered this blog when I was looking thru the pictures we took today on my Surgiversary. My sweet Husband came home from school in the afternoon today....and we first took Isabella to the park together...and then all went out to dinner!When we got home...I saw russ had taken a BUNCH of pictures of Isabella and I playing 'tag/chase' on the jungle gym playground....These pictures are soooo precious to me....they are not very good quality....but I love them! Another reason that drove me to WLS was I never wanted to take 'Bella to the park when she was little b/c I was afraid if she ran faster than me - that I wouldn't be able to RUN after her - to keep her safe and from danger! Now...I not only could do that - but, I can Run and PLAY!! Praise GOD....my daughter is going to have a Mommy that can play....I love that for her!
 I love this picture of us playing tag....and then there is more where SHE is chasing ME!! Today was such a wonderful
I love this picture of us playing tag....and then there is more where SHE is chasing ME!! Today was such a wonderful  day....and evening with my family.... PRAISE GOD for this surgery...and all the will power he's given me this year...and the success!
day....and evening with my family.... PRAISE GOD for this surgery...and all the will power he's given me this year...and the success! I've lost 143.6#'s in 12 months....
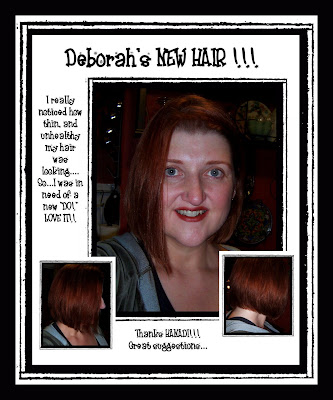
My New Hair...
Jan 24, 2007
I really love it...it's short...but still 'sassy!'
"To Diet....or Not To Diet...."
Jan 04, 2007
My NEW Favorite Quote:
Dec 31, 2006
I'm Just "Obese"....
Dec 23, 2006
I've been fat for soooo long....
So early on in my journey as I've done my personal appraisals I'd be very conscious of what the scale said. So much so that I put a ton on value on those numbers as well as the numbers that hung in the waistbands and necklines of my wardrobe.
Soooo...when "they" whoever "they are" came up with a new way to audit myself....I unconscously conceeded and took upon yet ANOTHER label that says: "Morbidly Obese"
Which brings me to -
Most of you know of my "scale addiction"....and the fact that I weight every other day....if not every day. Well...I haven't really checked the BMI scale lately - until tickerfactory started offering it as an option.
I just saw today....I'm no longer "morbidly obese" - I'm JUST "obese."
JOURNAL: December 20th - "8 Months PostOP"
Dec 20, 2006

 (You can click on each image for a Larger view!)
(You can click on each image for a Larger view!) 

POUCH RULES: Something for my personal reference
Dec 01, 2006
One of my SWEET friends from the RenewedReflections board posted this...and I never want to forget this information...I thought it could be important information here for other as well.... (sorry I'm not quoting who wrote it...but, it's not me...and its been VERY helpful!)
~ Deborah
________________________________________________________
INTRODUCTION: A common misunderstanding of gastric bypass surgery is thatthe pouch causes weight loss because it is so small, the patient eats less.Although that is true for the first six months, that is not how it works.Some doctors have assumed that poor weight loss in some patients is becausethey aren't really trying to lose weight. The truth is it may be because theyhaven't learned how to get the "satisfied" feeling of being full to lastlong enough.
HYPOTHESIS OF POUCH FUNCTION: We have four educated guesses as to how the pouch works:
- Weight loss occurs by actually "slightly stretching" the pouch with foodat each meal or;
- Weight loss occurs by keeping the pouch tiny through never everoverstuffing or;
- Weight loss occurs until the pouch gets worn out and regular eatingbegins or;
- Weight loss occurs with education on the use of the pouch.
PUBLISHED DATA: How does the pouch make you feel full?The nerves tell the brain the pouch is distended and that cuts off hungerwith a feeling of fullness.What is the fate of the pouch? Does it enlarge? If it does, is it becausethe operation was bad, or the patient is overstuffing themselves, or does thepouch actually re-grow in a healing attempt to get back to normal?For ten years, I had patients eat until full with cottage cheese every threemonths, and report the amount of cottage cheese they were able to eat beforefeeling full. This gave me an idea of the size of their pouch at three monthintervals. I found there was a regular growth in the amount of intake ofevery single pouch. The average date the pouch stopped growing was twoyears. After the second year, all pouches stopped growing. Most pouches ended at 6oz., with some as large at 9-10 ozs.We then compared the weight loss of people with the known pouch size of eachperson, to see if the pouch size made a difference. In comparing the largepouches to the small pouches,
THERE WAS NO DIFFERENCE IN PERCENTAGE OFWEIGHT LOSS AMONG THE PATIENTS. This important fact essentially shows that it isNOT the size of the pouch but how it is used that makes weight loss maintenancepossible.
OBSERVATIONAL BASED MEDICINE:The information here is taken from surgeon's "observations" as opposed to"blind" or "double blind" studies, but it IS based on 33 years of physicianobservation.Due to lack of insurance coverage for WLS, what originally seemed like aserious lack of patients to observe, turned into an advantage as I was ableto follow my patients closely. The following are what I found to effect howthe pouch works:
- Getting a sense of fullness is the basis of successful WLS.
- Success requires that a small pouch is created with a small outlet.
- Regular meals larger than 1 ½ cups will result in eventual weight gain.
- Using the thick, hard to stretch part of the stomach in making the pouchis important.
- By lightly stretching the pouch with each meal, the pouch send signals tothe brain that you need no more food.
- Maintaining that feeling of fullness requires keeping the pouch stretchedfor a while.
- Almost all patients always feel full 24/7 for the first months, then thatfeeling disappears.
- Incredible hunger will develop if there is no food or drink for eighthours.
- After 1 year, heavier food makes the feeling of fullness last longer.
- By drinking water as much as possible as fast as possible ("waterloading"), the patient will get a feeling of fullness that lasts 15-25minutes.
- By eating "soft foods" patients will get hungry too soon and be hungrybefore their next meal, which can cause snacking, thus poor weight loss orweight gain.
- The patients that follow "the rules of the pouch" lose their extraweight and keep it off.
- The patients that lose too much weight can maintain their weight bydoingthe reverse of the "rules of the pouch."
HOW DO WE INTERPRET THESE OBSERVATIONS?
POUCH SIZE:By following the "rules of the pouch," it doesn't matter what size the pouchends up. The feeling of fullness with 1 ½ cups of food can be achieved.
OUTLET SIZE: Regardless of the outlet size, liquidity foods empty faster than solid foods.High calorie liquids will create weight gain.
EARLY PROFOUND SATIETY: Before six months, patients much sip water constantly to get in enough watereach day, which causes them to always feel full.After six months, about 2/3 of the pouch has grown larger due to the naturalhealing process. At this time, the patient can drink 1 cup of water at a time.
OPTIMUM MATURE POUCH: The pouch works best when the outlet is not too small or too large and thepouch itself holds about 1 ½ cups at a time.
IDEAL MEAL PROCESS (rules of the pouch):
- The patient must time meals five hours apart or the patient will get toohungry in between.
- The patient needs to eat finely cut meat and raw or slightly cookedveggies with each meal.
- The patient must eat the entire meal in 5-15 minutes. A 30-45 minute mealwill cause failure.
- No liquids for 1 ½ hours to 2 hours after each meal.
- After 1 ½ to 2 hours, begin sipping water and over the next three hoursslowly increase water intake.
- 3 hours after last meal, begin drinking LOTS of water/fluids.
- 15 minutes before the next meal, drink as much as possible as fast aspossible. This is called "water loading," IF YOU HAVEN'T BEEN DRINKING OVERTHE LAST FEW HOURS, THIS 'WATER LOADING' WILL NOT WORK.
- You can water load at any time 2-3 hours before your next meal if you get hungry, which will cause a strong feeling of fullness.
THE MANAGEMENT OF PATIENT TEACHING AND TRAINING: You must provide information to the patient preoperatively regarding thefact that the pouch is only a tool: a tool is something that is used to perform atask but is useless if left on a shelf unused. Practice working with a toolmakes the tool more effective.
NECESSITY FOR LONG TERM FOLLOW-UP: Trying to practice the "rules of the pouch" before six to 12 months is awaste. Learning how to delay hunger if the patient is never hungry justdoesn't work. The real work of learning the "rules of the pouch" beginsafter healing has caused hunger to return.
PREVENTION OF VOMITING: Vomiting should be prevented as much as possible. Right after surgery, thepatient should sip out of 1 oz cups and only 1/3 of that cup at a time untilthe patient learns the size of his/her pouch to avoid being sick.It is extremely difficult to learn to deal with a small pouch. For the first6 months, the patient's mouth will literally be bigger than his/her stomach,which does not exist in any living animal on earth.In the first six weeks the patient should slowly transfer from a liquid dietto a blenderized or soft food diet only, to reduce the chance of vomiting.Vomiting will occur only after eating of solid foods begins. Rice, pasta,granola, etc., will swell in time and overload the pouch, which will causevomiting. If the patient is having trouble with vomiting, he/she needs toget 1 oz cups and literally eat 1 oz of food at a time and wait a few minutesbefore eating another 1 oz of food. Stop when "comfortably satisfied," untilthe patient learns the size of his/her pouch.
SIX WEEKS: After six weeks, the patient can move from soft foods to heavy solids. Atthis time, they should use three or more different types of foods at eachsitting. Each bite should be no larger than the size of a pinkie fingernailbed. The patient should choose a different food with each bite to preventthe same solids from lumping together. No liquids 15 minutes before or 1 ½ hoursafter meals.
REASSURANCE OF ADEQUATE NUTRITION: By taking vitamins everyday, the patient has no reason to worry aboutgetting enough nutrition. Focus should be on proteins and vegetables at each meal.
MEAL SKIPPING: Regardless of lack of hunger, patient should eat three meals a day. In thebeginning, one half or more of each meal should be protein, until thepatient can eat at least two oz of protein at each meal.
ARTIFICIAL SWEETENERS: In our study, we noticed some patients had intense hunger cravings whichstopped when they eliminated artificial sweeteners from their diets.
AVOIDING ABSOLUTES: Rules are made to be broken. No biggie if the patient drinks with one meal -as long as the patient knows he/she is breaking a rule and will get hungryearly. Also if the patient pigs out at a party - that's OK because beforesurgery, the patient would have pigged on 3000 to 5000 calories and with thepouch, the patient can only pig on 600-1000 calories max. The patient needs to just get back to the rules and not beat him/herself up.
THREE MONTHS: At three months, the patient needs to become aware of thecalories per gram of different foods to be aware of "the cost" of each gram.(cheddar cheese is 16 cal/gram; peanut butter is 24 cals/gram). As soon ashunger returns between three to six months, begin water loading procedures.
THREE PRINCIPLES FOR GAINING AND MAINTAINING SATIETY:
- Fill pouch full quickly at each meal
- Stay full by slowing the emptying of the pouch. (Eat solids. No liquids15minutes before and none until 1 ½ hours after the meal). A scientific testshowed that a meal of egg/toast/milk had almost all emptied out of the pouchafter 45 minutes. Without milk, just egg and toast, more than ½ of the mealstill remained in the pouch after 1 ½ hours.
- Protein, protein, protein. Three meals a day. No high calorie liquids.
FLUID LOADING: Fluid loading is drinking water/liquids as quickly as possible to fill thepouch which provides the feeling of fullness for about 15 to 25 minutes. The patient needs to gulp about 80% of his/her maximum amount of liquid in 15 to30 SECONDS. Then just take swallows until fullness is reached. The patientwill quickly learn his/her maximum tolerance, which is usually between 8-12oz.Fluid loading works because the roux limb of the intestine swells up,contracting and backing up any future food to come into the pouch. The pouch is very sensitive to this and the feeling of fullness will last much longerthan the reality of how long the pouch was actually full. Fluid load before each meal to prevent thirst after the meal as well as to create that feeling of fullness whenever suddenly hungry before meal time.
POST PRANDIAL THIRST: It is important that the patient be filled with water before his/her nextmeal as the meal will come with salt and will cause thirst afterwards. Beingtoo thirsty, just like being too hungry will make a patient nauseous. Whilethe pouch is still real small, it won't make sense to the patient to do thisbecause salt intake will be low, but it is a good habit to get into becauseit will make all the difference once the pouch begins to regrow.
URGENCY: The first six months is the fastest, easiest time to lose weight. By the endof the six months, 2/3 of the regrowth of the pouch will have been done.That means that each present day, after surgery you will be satisfied with lesscalories than you will the very next day. Another way to put it is thatevery day that you are healing, you will be able to eat more. So exercise as muchas you can during that first six months as you will never be able to loseweight as fast as you can during this time.
SIX MONTHS: Around this time, our patients begin to get hungry between meals. THEY NEEDTO BATTLE THE EXTRA SALT INTAKE WITH DRINKING LOTS OF FLUIDS IN THE TWO TO THREE HOURS BEFORE THEIR NEXT MEAL. Their pouch needs to be well watered before they do the last gulping of water as fast as possible to fill the pouch 15 minutes before they eat.
INTAKE INFORMATION SHEET AS A TEACHING TOOL: I have found that having the patients fill out a quiz every time they visitreminds them of the rules of the pouch and helps to get them "back ontrack." Most patients have no problems with the rules, some patients reallystruggle to follow them and need a lot of support to "get it", and a smallpercentage never quite understand these rules, even though they are quite intelligent people.
HONEYMOON SYNDROME: The lack of hunger and quick weight loss patients have in the first sixmonths sometimes leads them to think they don't need to exercise as much andcan eat treats and extra calories as they still lose weight anyway. We callthis the "honeymoon syndrome" and they need to be counseled that this is theonly time they will lose this much weight this fast and this easy and not towaste it by losing less than they actually could. If the patient's weightloss slows in the first six months, remind them of the rules of water intakeand encourage them to increase their exercise and drink more water. You cancompare their weight loss to a graph showing the average drop of weight ifit will help them to get back on track.
EXERCISE: In addition to exercise helping to increase the weight loss, it is importantfor the patient to understand that exercise is a natural antidepressant andwill help them from falling into a depression cycle. In addition, exercisejacks up their metabolic rate during a time when their metabolism after theshock of surgery tends to want to slow down.
THE IDEAL MEAL FOR WEIGHT LOSS: The ideal meal is one that is made up of the following: ½ of your meal to below fat protein, ¼ of your meal low starch vegetables and ¼ of your mealsolid fruits. This type of meal will stay in your pouch a long time and is good for your health.
VOLUME VS. CALORIES: The gastric bypass patient needs to be aware of the length of time it takesto digest different foods and to focus on those that take up the most spaceand take time to digest so as to stay in the pouch the longest, don't worryabout calories. This is the easiest way to "count your calories." Forexample, a regular stomach person could gag down two whole sticks of butterat one sitting and be starved all day long, although they more than haveenough calories for the day. But you take the same amount of calories invegetables, and that same person simply would not be able to eat that muchfood at three sittings - it would stuff them way too much.
ISSUES FOR LONG TERM WEIGHT MAINTENANCE: Although everything stated in this report deals with the first year aftersurgery, it should be a lifestyle that will benefit the gastric bypasspatient for years to come, and help keep the extra weight off.
COUNTER-INTUITIVENESS OF FLUID MANAGEMENT: I admit that avoiding fluids at meal time and then pushing hard to drinkfluids between meals is against everything normal in nature and not anatural thing to be doing. Regardless of that fact, it is the best way to stay fullthe longest between meals and not accidentally create a "soup" in thestomach that is easily digested.
SUPPORT GROUPS: It is natural for quite a few people to use the rules of the pouch and thento tire of it and stop going by the rules. Others "get it" and adhere to therules as a way of life to avoid ever regaining extra weight. Having a support group makes all the difference to help those that go astray to be reminded of the importance of the rules ofthe pouch and to get back on track and keep that extra weight off. Support groups create a "peer pressure" to stick to the rules that the staff at the physician's office simply can'tcreate.
TEETER TOTTER EFFECT: Think of a teeter totter suspended in mid air in front of you. Now on theleft end is exercise that you do and the right end is the foods that youeat. The more exercise you do on the left, the less you need to worry about the amount of foods you eat on the right. In exact reverse, the more you worry about the foods you eat and keep it healthyon the right, the less exercise you need on the left. Now if you don'tconcern yourself with either side, the higher the teeter totter goes, whichis your weight. The more you focus on one side or the other, or even bothsides of the teeter totter, the lower it goes, and the less you weigh.
TOO MUCH WEIGHT LOSS: I have found that about 15% of the patients which exercise well and had between 100 to 150 lbs to lose, begin to lose way too much weight. I encourage them to keep up the exercise (which is great for their health) and to essentially "break the rules" of the pouch. Drink with meals so they caneat snacks between without feeling full and increase their fat content aswell take a longer time to eat at meals, thus taking in more calories. Asmall but significant amount of gastric bypass patients actually gounderweight because they have experienced (as all of our patients haveexperienced) the ravenous hunger after being on a diet with an out ofcontrol appetite once the diet is broken. They are afraid of eating again. Theydon't "get" that this situation is literally, physically different and that theycan control their appetite this time by using the rules of the pouch toeliminate hunger.
BARIATRIC MEDICINE: A much more common problem is patients who after a year or two plateau at alevel above their goal weight and don't lose as much weight as they want. Becareful that they are not given the "regular" advice given to any averageoverweight individual. Several small meals or skipping a meal with a liquidprotein substitute is not the way to go for gastric bypass patients. Theymust follow the rules, fill themselves quickly with hard to digest foods,water load between, increase their exercise and the weight should come offmuch easier than with regular people diets.
SUMMARY:
- The patient needs to understand how the new pouch physically works.
- The patient needs to be able to evaluate their use of the tool, compareitto the ideal and see where they need to make changes.
- Instruct your patient in all ways (through their eyes with visual aids,ears with lectures and emotions with stories and feelings) not only on howbut why they need to learn to use their pouch. The goal is for the patientto become an expert on how to use the pouch.
EVALUATION FOR WEIGHT LOSS FAILURE: The first thing that needs to be ruled out in patients who regain their weight is how the pouch is set up.
- The staple line needs to be intact;
- Same with the outlet and;
- The pouch is reasonably small.
- Use thick barium to confirm the staple line is intact. If it isn't, thenthe food will go into the large stomach, from there into the intestines andthe patient will be hungry all the time. Check for a little ulcer at thestaple line. A tiny ulcer may occur with no real opening at the line, whichcan be dealt with as you would any ulcer. Sometimes, though, the ulcer isthere because of a break in the staple line. This will cause pain for thepatient after the patient has eaten because the food rubs the little opening of the ulcer. If there is a tiny opening at the staple line, then are operation must be done to actually separate the pouch and the stomachcompletely and seal each shut.
- If the outlet is smaller than 7-8 mill, the patient will have problemseating solid foods and will little by little begin eating onlyeasy-to-digestfoods, which we call "soft calorie syndrome." Thiscauses frequent hunger and grazing, which leads to weight regain.
- To assess pouch volume, an upper GI doesn't work as it is a liquid. Thecottage cheese test is useful - eating as much cottage cheese as possible infive to 15 minutes to find out how much food the pouch will hold. Itshouldn't be able to hold more than 1 ½ cups in 5 - 15 minutes of quickeating.
If everything is intact then there are four problems that it may be:
- The patient has never been taught the rules;
- The patient is depressed;
- The patient has a loss of peer support and eventual forgetting of rules,or
- The patient simply refuses to follow the rules.
- LACK OF TEACHING: An excellent example is a female patient who is 62 years old. She had theoperation when she was 47 years old. She had a total regain of her weight.She stated that she had not seen her surgeon after the six week follow up 15years ago. She never knew of the rules of the pouch. She had initially lost50 lbs and then with a commercial weight program lost another 40 lbs. Afterthat, she yo-yoed up and down, each time gaining a little more back. Shethen developed a disease (with no connection to bariatric surgery) which weakenedher muscles, at which time she gained all of her weight back. At the timeshe came to me, she was treated for her disease, which helped her to beginwalking one mile per day. I checked her pouch with barium and the cottagecheese test which showed the pouch to be a small size and that there was noleakage. She was then given the rules of the pouch. She has begun animpressive and continuing weight loss, and is not focused on food as shewas, and feeling the best she has felt since the first months after her operation15 years ago.
- DEPRESSION: Depression is a strong force for stopping weight loss or causing weightgain.A small number of patients, who do well at the beginning, disappear for awhile only to return having gained a lot ofweight. It seems that they almost on purpose do exactly opposite ofeverything they have learned about their pouch: they graze during the day,drink high calorie beverages, drink with meals and stop exercising, eventhough they know exercise helps stop depression. A 46 year-old woman, oneyear out of her surgery had been doing fine when her life was turned upsidedown with divorce and severe teenager behavior problems. Her weightskyrocketed. Once she got her depression under control and began refocusingon the rules of the pouch, added a little exercise, the weight came offquickly. If your patient begins weight gain due to depression, get him/herinto counseling quickly. Encourage your patient to refocus on the pouchrules and try to add a little exercise every day. Reassure your patient thathe/she did not ruin the pouch, that it is still there, waiting to be used to helpwith weight control. When they are ready the pouch can be used once again tolose weight without being hungry.
- EROSION OF THE USE OF PRINCIPLES: ome patients who are compliant, who are not depressed and have intactpouches, will begin to gain weight. These patients are struggling with theirweight, have usually stopped connecting with their support groups, and havebegun living their "new" life surrounded by those who have not had Bariatricsurgery. Everything around them encourages them to live life "normal" liketheir new peers: they begin taking little sips with their meals, and eatingquick and easy-to-eat foods. The patient will not usually call theirphysician's office because they KNOW what they are doing is wrong and KNOWthat they just need to get back on track. Even if you offer "refreshercourses" for your patients on a yearly basis, they may not attend becausethey KNOW what the course is going to say, they know the rules and how theyare breaking them. You need to identify these patients and somehow get themback into your office or back to interacting with their support group again.Once these patients return to their support group, and keep in contact withtheir WLS peers, it makes it much easier to return to the rules of the pouchand get their weight under control once again.
- TRUE NONCOMPLIANCE: The most difficult problem is a patient who is truly noncompliant. Thispatient usually leaves your care, complains that there is no 'connection'between your staff and themselves and that they were not given the time andattention they needed. Most of the time, it is depression underlying thenoncompliance that causes this attitude. A truly noncompliant patient willusually end up with revisions and/or reversal of the surgery due to weightgain or complications. This patient is usually quite resistant tocounseling. There is not a whole lot that can be done for these patients as they willfind a reason to be unhappy with their situation. It is easier to identifythese patients BEFORE surgery than to help them afterwards, although Ireally haven't figured out how to do that yet. Besides having a psychological examdone before surgery, there is no real way to find them before surgery and Iusually tend toward the side of offering patients the surgery with educationin hopes they can live a good and healthy life.
________________________________________
JOURNAL: 7 mos. PostOp
Nov 24, 2006
(click on the pictures for larger view)
Wow...it's hard to believe sometimes that it's been 7mos.....and then again, that time is so short, for the amount of weight I've lost. My new total is 111#'s....I'm loosing at a considerably slower rate now...which is good/bad.
Good, b/c I'm loosing at a normal rate....BAD, b/c I'm used to the pounds just dropping off...and now I have to work for it...and be patient for the results.
I'm glad it was fast at first b/c I just KNOW me....if it wouldn't have worked this way - I would've given up like so many other times I tried to loose weight! It never was successful. This has been a transition...I'm not gonna say "hard" - b/c that is a story to make this choice a little more dramatic. It is what it is...and I'm glad for my choice to have weight loss surgery. 
Boy, do I feel amazing! Now if the last 72#'s could come off easy... but, something tells me it won't be that easy... I'm gonna have to work at it - the mere "mortal way!" LOL.