Rosalind G.
My WLS and PS Journey
Jan 11, 2008
I was brought up learning the principles of good nutrition. I just can't seem to control my apetite. I've been on Jenny, Weight Watchers, Atkins. I've done Pilates for 5 years, at my peak Pilates 3xweek with yoga 4xweek. I am a fat lady with muscles. If I don't lose weight, I'll never see my grandchildren. My maternal family has a stroke history, although they were all vegetarians.
I have not felt hope about my weight in years until I started to study this website a few days ago. I'd been studying bariatric surgery for a few months when I recently met a woman who had surgery 5 years ago and she's just beautiful today after losing 130#.
To think that I could once again climb mountains as I did with my older children when they were young, that I could play soccer and dive for baseballs with my younger ones would be a dream come true, not to mention fit in an economy class airplane seat comfortably.
I am so ready to have this surgery. I have begun to pray for God's guidance in this.
September 6, 2003
A good friend had WLS 5 years ago and lost 130 lbs. She loved her surgeon and referred me to Dr. Sheila Clayton in Pasadena, CA. This was my first entry into the world of bariatrics. I was surprised that I wouldn't see the surgeon until after I had gone to the required lecture and that I would havae to pay $250 out of pocket for a psychological evaluation. If I passed that, then I would be able to meet with the surgeon. When I asked what would happen if I paid the money, was "accepted", then met with Dr. Clayton and decided we weren't a good match, I was told that by the time I got that far they assumed I would want to proceed with the surgery. This is definitely a different world. Uncomfortable with this ritual, I decided to look elsewhere. Also, Dr. Clayton doesn't accept HMOs.
September 11, 2003
I went to a symposium given by Dr Jamshid Nagerian and had a few minutes before it began to speak with members in his support group. They were a positive and humerous group. Dr. Nagerian's lecture was very informative. He had a soft and gentle voice and seemed to have a sincere desire to help his patients change their lives. However, he doesn't accept HMO's either. Their system sounded wonderfully streamlined, taking a lot of work and worry away from the patients. I have the option to change my insurance and return in January 2004. I decided to think about this.
September 18, 2004
I called my insurance company, finally putting the cart behind the horse. I was told they cover WLS when medically necessary. They referred me to my IPA. I spoke with a wonderful woman who told me everything I needed to document my case, "Everything and anything."
Three days ago I saw my PCP. He was decidedly underwhelmed with my idea for surgery. He said he'd write the authorization request because I "demanded" he do so. I laughed and told him I was merely "gently urging" him. He is afraid of the dangers involved. Today,I saw my psychiatrist and he is also afraid of the mortality rate. He gave me a prescription for Topamax. He had a patient who lost 120lbs in a year taking this. He said there's no guarantee it will always perform like that, but it provides a sense of satiety and most people lose a good amount of weight. So I ask myself, do I try yet again? Do I wait and see? Or have I had it? What is the reasonable path? I'm just so weary of this cycle of hope and despair.
At any rate, I discovered that one of the surgeons I had initially researched is in the contracting group with my IPA. Their seminar is Oct. 1st. So, more later on this rather wierd journey.
One final note. I feel a certain amount of guilt complaining about my weight when I read here of so many others who have struggled with hundreds of pounds more than I have. So, I write this respectfully and apologetically to those who have gone before me, who had so much farther to go than I.
September 26, 2003
I just realized that I DO have shame about my obesity. I never characterized this reluctance to go my children's school functions, or to parties, or virtually all other social functions because I'm so heavy, as shame, but that's exactly what it is. I don't practice baseball or soccer with my boys because it's just too hard to run.
I thought I had made up my mind about the type of surgery I wanted, then I read some profiles on the DS forum, reread info on surgery types and began to feel less certain about RNY. Now, BPD/DS sounds like it might be better. Conundrum.
Gained a pound. Hah. I have an important meeting in November in Washington, DC. I've gained 35 lbs since I last saw these people in May. How can I face them? I want surgery yesterday.
September 30: Tomorrow night is the Symposium with Dr. Lourie (or Dr. Troy LaMar) at Huntington Memorial Hospital in Pasadena, CA. They do the Rny. I missed the DS symposium that Dr. Anthone held on Saturday and the next one won't be until the end of October. Dr. Anthone is booked into February 2004. I'm doing more research on BPD/DS, but happy to attend the RnY symposium.
I have to push myself up from the chair now. What a hideous disability this is. How could anyone justify being "Big and Beautiful" when it's impossible to walk half a block uphill without gasping for breath?
October 1: Feast or famine. Discovered a symposium in Ventura on DS by the Drs. Rabkin of San Francisco and chose to go there instead of the RnY lecture by Lourie and LaMar. The meeting was a real education and I'm convinced the DS is best for me. I also went with my son's girlfriend. I guess he's learned to love the big and the brave. Dr.Rabkin didn't actually speak and it was difficult to get to him through the adoring crowd of his post-op patients after the talk. His RN is a very caring person and seems to know as much as there is to be known about insurance and the surgery. Also, I brought my son's girlfriend along.
Two weeks later, Allie and I got to the Arcadia meeting given by Lourie and LaMar. They touted the gold standard RnY, ran a video of the actual lap surgery, and took one question per person after the lecture. It was a large crowd. What can I say? Well, I thought LaMar was quite dashing, but my mind's made up about the DS. However, it was important for Allie to learn more about the RnY.
October 24: All of my boys are spending the night with a good friend tonight and I've had time to go the movies and sit down here for awhile reading other's journeys. Tomorrow morning Allie and I will go to a symposium by Dr. Peter Crookes from USC/University Hospital. Dr. Anthone has left the practice there and I understand that Crookes is leaping into the breach. My R.N. daughter, who works the ICU step down unit, says he's probably the nicest doc in the hospital. I asked her if he were married, you know, a widow wonders. . . .
I emailed the obesity attorney on this website a few days ago. I don't see any reason to wait until I've been denied more than once. I'm also switching to BS/CalPers PPO so that I can have the freedom to choose not only my own surgeon, but other physicians, as well.
Studying the BS/CalPers HMO website this week,I learned that subscribers are allowed a non-referred consultation for a second opinion with an "Access+" specialist. I don't want to make a move at this point, however, without speaking to the attorney first.
Some wonderful person on this forum, has a super Profile filled with some links I'd never seen before. She had an apnea quizz that I took resulting in a score of 40. Just like my BMI. Apparently, that puts me in the high risk category. So, I made an appointment with my PCP for next week.
If he will actually refer me (a process he seems to find excruciatingly difficult) for a formal exam, I think this will be another dot on the i of another insurance criterium. I'm also going to share with him, and everyone right here, that I have stress incontinence which I thought was just part of "age".
I have an old lab order he wrote for a complete blood workup that I'm having done on Monday, so we can both see just how ghastly is my bad cholesterol. I've also noticed a rather wheezy, tight feeling in my chest and it hurts to breath in deeply. I'm asking that that also be carefully checked because I've read one problem with MO is a sort of chronic bronchitis. My hypertension med is working, but BP is still higher than I'm comfortable with. Edema still plagues me.
This is really a wierd experience, writing all of this for people I don't know. Rather like a letter in a bottle. It's clearly fulfilling some cathartic need.
10/24: Went to seminar given by the USC/University Hospital bariatric surgeons. Brilliant group, all clinical professors. Huge audience there. Must have been 100 people. Dr. Nemir Katkhouda is the only one of the group that does the lap DS.
10/28: Scheduled an appointment with Dr. Nemir Katkhouda of USC/University Hospital for first week in November. I've decided to switch from Blue Shield CalPers/HMO, to BC/PPO PersCare to have freedom of choice. The bariatric surgeons with the HMO are all wonderful doctors, but they only perfrom the RnY, and maybe the VBG, and I have chosen--if Dr Katkhouda agrees-the lap DS.
I chose to pay cash for the initial consult just so that I can get my feet in the door, eventhough if I waited until January, I don't think I'd have anything to pay other the minimal copay. I'm doing a lot of number crunching to decide between CalPers PersChoise or PersCare. The price difference is marked. I wish the doctor were contracted with the HMO I have.
Progress is at hand.
December 19, 2003
I've posted two long entries and lost both because of some stupid computer glitch. At some point I'll fill in the gaps, but here's where I'm at now:I've been moving so fast, I'm going slower. This will be the third Christmas for the boys and me without our beloved daddy. I thought I was handling it pretty well, even if I haven't been able to get it together to get a tree, but I've had to face that it is hard and here we go again--it hurts, we'll never be the same again, but, as we always have, we'll pull through with our hearts aching. We all feel better now than 2-1/2 years ago, that agonal pain is over, but I did hope that finally I wouldn't cry again that he's not here with us.
Maybe I'm going into another wretched grief time. I just can't seem to get anything done. Forgot to take an important field trip permission slip in to 10 year old's teacher, couldn't make it to "lunch with a parent" today with the 7 year old, couldn't make the bank deposit all week so couldn't cover the check for the painter who did my garage door. So stupid when I had the money, but not the energy to get to the bank. Only two rolls of toilet paper left in the house because I can't get it together to go to Smart and Final because I won't cross a picket line.
And I had my sleep apnea test last night at Huntington Memorial Hospital in Pasadena which should have been a good thing, but I was so tired when I got home in the morning, that after driving child to school, I came home, flopped on sofa, and didn't wake up until I was too late for the next big test, my cardiac treadmill stress exam. I'm just dropping one ball after another.
I don't think I'm depressed, but I can't even seem to help my children with the basics, like homework, because I'm just so weary. My BMI doesn't seem high enough to be so utterly incompetent. I can't walk a block uphill without panting and sweating like a stevedore. I get home from somewhere and sit in the car for a moment just spacing out.
I should have put this in my profile. Basta. I'm off to look at my inspiration, all of the B&A photos.
I'm glad I can do this at night, speak with unknown friends, invisible, miles away, but so truly caring.
Hah! I just reread my intro above. I've gained 30 pounds since then. I'm up to 255.5. No wonder I can't walk uphill, or roll over without a major push up.
December 28, 2003
I never intended to have such a gaping hole in my profile, but twice I sat down and spent a couple of hours updating, only to hit some button that I shouldn't have on my laptop, and bam! everything was gone.
These are the pertinent details of my progress. I chose to go with PersCare BC/PersChoice PPO. PersCare is the health benefits division: Public Employees Retirement System (PERS) for the fine state of California. This will be effective 1/1/04, just a few days from now. It seems that with 2004, BC has stated they will allow WLS for medical necessity. In an odd sort of backwards way, they have listed the surgeries they won't cover, which is all WLS, but they HAVE included DS in their list. Therefore, as I understand it, they will authorize any of these when medically necessary. I'm paying more for my premiums, and will probably return to the HMO next year, but the PPO should make the authorization process smoother.
For about two months (October, November) I wavered in my decision to have open or lap DS, but I always knew I wanted the DS and espcially that it be done lap. With three little boys, I need the faster recovery lap surgery offers. Behind my indecision was the fact that Dr. Crookes only does DS open and I really wanted to be in USC/University Hospital where my daughter works in the IC Stepdown unit.
It seemed my only choice was to go open, or go to San Francisco with Dr. Rabkin. Then I found a more local doctor who has begun doing lap DS. I posted a note in CA message board and a dear and very informed member emailed me to do further research on him. I did and found 3 or 4 complaints about very slow weight loss, and although he was very caring, he really didn't address some serious issues.
Back to the idea of a northerly trip to see Rabkin. I called the office and discovered I could be seen early January at their Ventura office for the Pre-op consult. That saves me about 5 hours driving, or $300 in airfare.
Meanwhile, my weight from first posting my profile rose from 230 pounds to 255.5! Tired of the endless fight, I just gave up all attempts at control and ate whatever I wanted, whenever I wanted until I finally began to feel so nauseous in the morning from eating late at night, that I couldn't eat breakfast.
For some odd reason, my weight has begun to creep back down and now I'm around 247-249. I think I got sick of chocolate candy and when I stopped eating 2 large Snickers bars a day, that helpled. LOL.
I haven't gotten the results because it was done the week before Christmas, but the oxygen felt wonderful as I drifted off to sleep during the test.
I've also had my blood work done and discovered I have high bad chloesterol.
When I went in to talk with my PCP about the apnea issue and the need for a treadmill stress test, I brought with me quite a packet of info I'd downloaded on bariatric surgery, DS procedure, Dr. Rabkin, and a form letter from Dr. Rabkin introducing himself to my PCP. Low and behold, he told me he had several patients who had had WLS and he was very happy with their results. THEN he said he thought I was a good candidate!!!I jumped up and hugged him.
I'm not sure what changed his mind about me, perhaps it was my weight/diet history I faxed him after the visit when he told me he didn't think I was an appropriate candidate. Maybe it was my ever upward weight gain, but whatever it was he's on my side now.
My psych eval and cardiac stress test are this week, just a few days before my Initial Consult. I am hoping they will have the results ready for me to take along.
Were it not for all of the wonderful AMOS profiles and the message boards, I wouldn't have known how important it is to line up all of this important work.
Barbara Metcalf, RN, the Program Director, has been very positive and helpful through email and phone calls. She said they will preapply and perhaps we can get an earlier date.
I remain overly tired and find it so difficult to even want to do anything outside.
That's all for now folks. Thanks for listening. . .
January 14, 2004
I met with Barbara, the program director for Dr. Rabkin, last week. Two days later, I had my psych eval with Dr. Bales, also in Ventura. Both said they thought I'd benefit from the surgery.
All necessary specialist testing has been completed. My psychiatrist will speak with Dr. Bales about the procedure, medication issues, etc.
So here I sit, one chubby chica waiting for the wheels to begin their grind.
Ah, but what of those wretched holidays, days of darkness for widows and their young children... The first of December I was thinking how great and pure and complete was my joy in these young lives so dependent on me, then day by day, the sun shone less brightly. By Christmas, I had begun slowly slide into the darkness of despair. After the first of the year, I became so weary I could only think about sleep, rest, get the two oldest to school, come home, drink 2 huge cups of coffee, wait for babysitter, go to bed. Nothing got done. I paid a few bills, and that was as close as I got to being even remotely in control. With money in the bank, I left other bills idle in the "urgent" folder that was supposed to help me prioritize my life. Thank heavens, my mortgage is automatically deducted.
Faithfully, taking my psych meds I began to wonder (talk about slow witted)could I be depressed???? Sleep, sense of failure, withdrawal, impatience, unbearable weariness??? You'd think by now I'd know what's happening. Last night I was watching TV and saw a commercial for an antidepressant. It listed the symptoms--all of which I well knew, but seemed to have forgotten--and the old "ah hah" button was pushed. This morning, I called my kind psychiatrist and upped the dose on one.
So what in the world does this have to with WLS??? WOuldn't it be just grand to learn after I've lost weight, that I might not get so sick? Can't believe it's possible, but I've read about it here.
My weight is up to 256.5 on my scale. I've read the bios of others who lost a hundred or more pounds to reach this weight, and how wonderful they've felt. I suppose this is as relative as everything else. I twist my body, a contortionist getting out of bed!!! I stuck in a chair yesterday!! How in the world are we supposed to even be truly hygienic if we can't effectively reach our nether parts? For crying out loud, I used to ski! I think I even laughed once upon a time.
I write of weariness, and look, here it is 1AM. I've been trying to get in bed by 11PM for past two nights and found I was actually able to not take a nap. Ah, tomorrow really is another day.
January 17
The timelessness of waiting without expectation:
The Zen of Insurance
Hope is the perfect state of being with intrinsic reward.
January 31
No surprise, BC denied request for DS surgery as they considered it "experimental". Dr. Rabkin's office is sending an appeal packet. Surgery would have been approved if I wanted a RnY, but I don't. I'll complete appeal, include my own letter, photo, and ABS statement on DS, along with other scientific literature. I'll also present the unique query if they'll pay the same fee for RnY, I'll make up the difference my self. I'll also call CalPers in Sacramento and speak with someone in their healthcare divison. CalPers is the largest employer in California. We'll see.
February 1
Yahoo's DS forum is a great resource for handling insurance problems. I found the most profound appeal letter I've ever read. The scientific documentation was exceptional. It was reasonable,logical, and direct in detailing the choice of DS over other WLS. I'm returning there tomorrow to update the resources this woman used, as it was written in 2002 and there has been even more published since then.
I suppose the upside of this is that BC didn't deny me surgery, just that procedure. Ever onward.
Oh, yes. Looks like I've gained another pound. My daughter said I've got to get back to the gym and hit the treadmill for just 5 minutes to get started. I live in a hilly area and the streets are too challenging for me now.
April 21, 2004. Time for what appears to be my quarterly update.
Initial appealed was denied March 31st by BC as DS was "investigational/experimental". I am now working on cover letter for my request for External Medical Review by CalPERS. If that fails, I go to DoI. These denials seem to come fairly quickly. It is rather hard to understand how a 20 page document (including a 3 page bibliography with 46 citations) could be carefully analyzed and denied 4 business days later. I doubt it landed in the reviewing doc's hands on 3/25, the date BC stated they received the appeal. Maybe the next day, the26th (a Friday).
At least I got a speedy reply. I was out of town for Easter break and the denial came while I was gone, then it took me a week to get caught up on family business. I think I'll have this packet in the mail, certified, return receipt, by tomorrow. Then I ought to know in a couple of weeks (if BC proves true to form) and I can plunge forward with DoI. Somebody along the way HAS to read this documentation!!!!!!!
June 3, 2004 (copied from a post to DS forum)
Can there really be 4 rounds in the ongoing tournament, me against them? With the 5th and 6th dark shadows ahead of me?
Warning! Potentially boring reading.
1st: Request for authorization denied by BC PersChoice (CalPers). 2/2004
2nd: Appeal denied. 3/31/2004
3rd: Appeal reopened 4/2004 because BC based their denial on my fax that stated I was opening the appeal process in which I listed in 4 sentences the basis for the appeal. They then received my 17 page letter, 3 page bibliography, and supporting data and honorably realized their mistake. Not that it changed their corporate mind.
3rd Appeal also denied. Surprise! In spite of my reasoned and scientific exposition of the facts about the DS, BC continued to maintain the DS' "investigational" status and cited the terrible peril of its malabsorption factor.
4th: Request for External Independent Review mailed by surgeon's office to BC 5/25/2004, but not received by 6/3/2004.
Paranoia my constant companion, I wait no longer and today ask surgeon's office to fax paper work to RN who initially reads the appeals. I think she gives her opinion to the doc who signs the form denial.
She who hesitates is lost. Tide and time wait on no morbidly obese person.
This aforementioned RN is very kind, soft spoken and caring. But, guess what? She had the RnY in January after a long period of research. She asked if I had a back up plan. Other than shooting myself, I said I was determined to have the DS.
Unconscious bias? Or a deep understanding of the rigidity of BC policy? I know she really wants to help me. She gave me her direct phone and fax numbers. She said she carefully read all I had written.
How, I ask, can any sentient being read all the documentation I had and not see the light of reason??? Do you think the facts even matter to the insurance companies?
I see Amy Olivas won at the point of IER, and that's what I'm hoping for.
June 5
Frustration making me just plain perspire too much, I called Jack. Jack Slade that is. His voice has a NYC edge making it tough. Slade, the attorney whose arms long enough to box with insurance companies, the fatcat corporate gods of greed.
We're meeting on the 8th. I'll have my check in hand along with all of my research and letters.
Slade said this could take up to 3 months. We'll see.
June 29
Make that Larry Slade. Good grief.
BC denied my request for independent examinor. So what. I can appeal directly to CalPERS and that paperwork goes out tomorrow. If they deny, it's DoI. Mr Slade has prevailed against BC for reimbursement. That's where we're going now. Who knows? Maybe the corporate fatcat pigs will come to their senses and acknowledge the advances made by science with the DS.
I have decided to self pay. I've scheduled my date with Dr Robert Rabkin in San Francisco for August 16. I'll go up on the 12th for pre-op details.
My daughter gave me a 7 pound 8 oz gift yesterday. And I'm pretty pleased right now. Alexandra Elizabeth. Has a ring to it, don't you think? Her 3 uncles, aged 3, 7 and 11, are pretty excited, too. Ah, a girl again . . .
JANUARY 25, 2005
My, how time flies when you're getting thin. I haven't updated because everytime I thought I should, it seemed like I had so much to say, I'd be typing all night.
Therefore:
Synopsis:
SURGERY was moved up to August 3, 2004. The best day in my life with the exception of the births of all my children and my marriage to my late husband.
The Journey begins in the office of Dr. Rabkin. In all 246 lbs of glory. Check out the ubiquitous spots on blouse. Where else was spilled food to go? Certainly not my nonexistent lap.

Dr. John Rabkin performed the DS at St Mary's in San Francisco. Piece of cake. I walked to the bathroom a couple of times that day, started laps down the hallways the next morning, by that evening I was climbing up and down the mini-steps the floor had. My room had a beautiful view, my morphine pump did the trick, and I said adios on day 3.
RECOVERY
I stayed with a post-op DS patient for 2 or 3 nights then moved to a hotel in San Francisco--to be closer to Macy's. I only needed about 4 vicodin after I was discharged from the hospital.
As an out-of-towner, I had to remain in SF for 10 days p/o and I loved it. The hotel chef prepared tiny portions of fabulous food for me. My first dinner was 2 large scallops in an exquisite garlic and white wine sauce. I was able to eat 1/3 of 1 scallop. I loved it. I paced in my room for exercise, read, and by day 5, walked to Macy's.
There was a terrific sale going on and I decided I'd come back and do back-to-school clothes for all my boys. It was a downhill walk from the hotel, which made it an uphill walk on the return. Slow, slow, sometimes wins the race. That night I was really, really tired and dozed on and off the next morning. By afternoon, I was ready to hit the sale. Before I left, I threw away 3 dresses I'd brought with me. They were already too large.
I bought all the kids' clothes, saved 40 to 60%. With so many bags, I needed a taxi and a Macy's clerk carried them outside and over to the taxi stand. That's service.
By the time I left for home, I'd lost 15#. At home, the boys were relieved to see that I wasn't thin. They had imagined I was going to come home a changed woman. Well, I was, but not quite as they thought.
EXERCISE
My backyard is sloped so I used the steps down to the bottom as an exercise launch in the beginning. I'd go up and down for 15 minute segments. I tried to get in 2 sets a day.
By week 6, I joined the local Y and started working out on the Cybex machines and Life Cycle. I'd take the 3 year old to swim class there, scurry over to the gym for half an hour, pick him up, dry him off and take him to their child care center and work out for another hour. Eventually, I started going in at 8AM after dropping the older boys off at school and that's still my pattern. I shoot for 5xweek, but usually only make 3-4. I feel so much better when I go.
I NEVER thought I'd say I enjoy exercise or that I could wish I had more time to spend at the gym, but that's how I feel these days.
This has paid off because I've had very little muscle mass loss.
October 2004 with 4 of the 5 boys. Note the bottle of ProteinIce in my hand. Taken at beautiful Descanso Gardens, La Canada, CA

SIDE EFFECTS
I've had absolutely no bad side effects. No diarrhea, no "accidents", no food intolerance, very little problem with gas unless I eat a few bites of, for example, banana nut bread.
My lap incision healed perfectly, although my navel looked like the nose of a creature from the dark side for awhile.
DIET
Protein drinks sustained me the first 3 weeks, or so. I ate eggs, fish, some roast beef, really just about anything, just not very much, so I had concerns about meeting the minimal 60gr mark.
Today, I really do eat any and everything. I'm buying much more expensive cuts of meat because a)they taste great and b)I usually get at least 3 meals out of a Porterhouse or T-bone steak.
For the first 4 months, I was rigid about no carbs and then Barbara, Dr Rabkin's wonderful RN, said I might be losing a little too fast so I should begin to include fruit and fruit juice. I thought what a WONDERFUL problem to have.
WEIGH-INs
I haven't wanted to obsess about my weight. I did that for years and look where it took me. Weighing only at follow-up appointments seemed like a good way to manage this and for the most part, I've been successful. I weighed when I came back from a follow-up to calibrate my scale with the doctor's and I've weighed a few times since then because the suspense was killing me.
BLESSINGS
I was off both hypertensive medications before I left the hospital. My B/P is normal for the first time in years. By the 3-1/2 month mark, my PCP couldn't believe my labs. He was sure the lab had made an error. My bad cholesterol had dropped from 300+ to 122.
My hips don't hurt at night when I sleep on my side. I can walk without the pain bringing me to a stop after a few steps. I can lift and carry my 4 y/o and not gasp for breath. I can get off the sofa without grunting and pushing myself up. I can walk in a hurry from the house to my car without gasping for breath by the time I'm behind the wheel.
Perhaps the greatest blessing is the fact I feel comfortable returning to volunteer at church and at the boys' school. I had gotten so fat, I couldn't bear to face people. I had virtually stopped going to church and that meant I wasn't taking the boys, either. I didn't go Family Camp with the church last year because I knew I couldn't participate in any of the physical activities and that even going up and down the stairs to our room would be awful--if we ended up on the 2nd floor.
Over Christmas break I took my 4 boys, the 3 little guys and my adult son, to Kauai. In a million years I wouldn't have gone anywhere that required a bathing suit before this surgery. We even camped out for 2 nights. I never would have been able to manage that before.
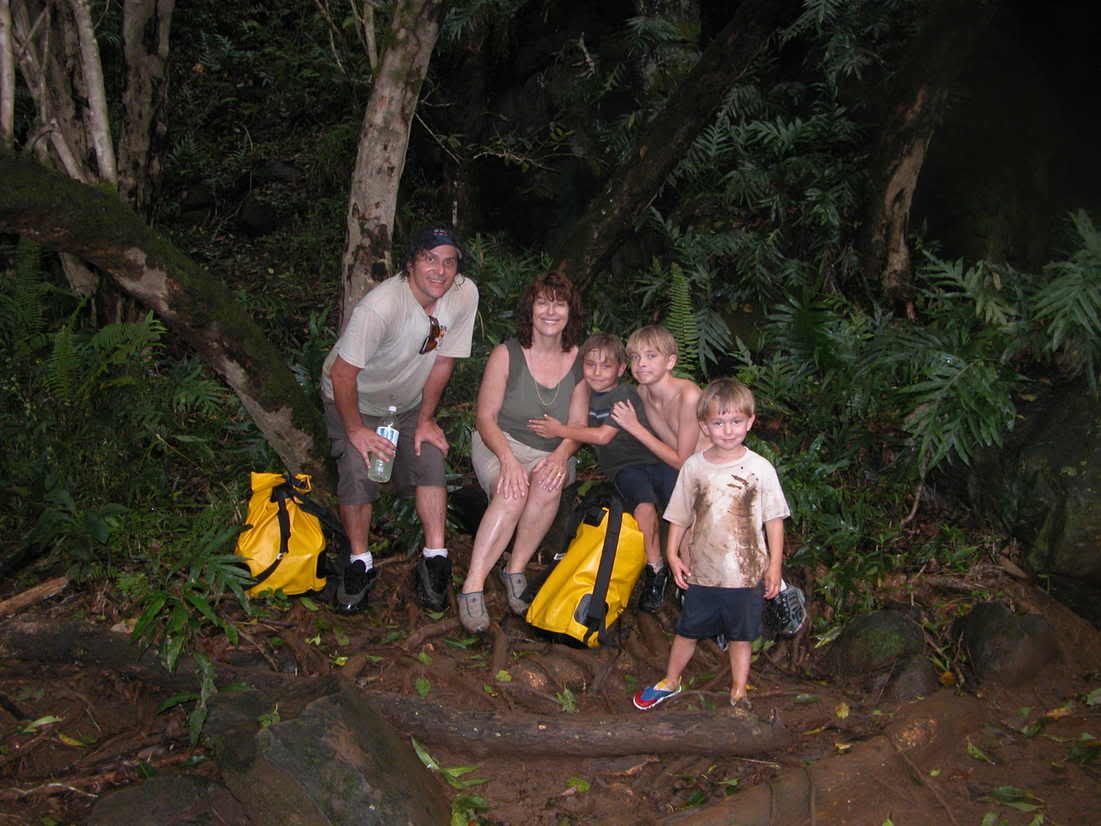
Sorry, no bathing suit shot, but here are 4 of the 5 boys and I in Kuaii, December 28, 2004. Muddy and happy.
In February, over Presidents' Day weekend, the boys and I are going with a small group from church to an orphanage in Tijuana that we work with. I am so happy that I am free at last to be able to serve in this way.
Through this entire process, pre-op and then post-op, I feel I have formed some real relationships with people on the DS message board. These are folks who have walked the same walk, cried the same tears, and rejoiced with me and each other over every victory.
I am so grateful for the support I've found here, and for this life saving surgery. I praise the Lord for the gifts he has given to the medical science that brought this possibility to us, and for the gifts of brilliance and skill he has granted those who saved our lives.
Two days ago, I put down a deposit for the obesityhelp.com Alaska cruise scheduled to depart Seattle July 30. I'm going alone, dropping the boys off in Portland to stay with family (that is, if the family can actually face 3 little boys), and then flying on to Seattle. It's expensive, but, you know, what in the world do I ever do for Rosalind? Even this surgery was primarily done so that I could live to see all of my children graduate from high school, not to mention college and grad school. I have some guilt about the money; I know it's not terribly responsible and that I really need to have the entire wrought iron fence painted; the dry rot on the eaves fixed and the house treated for termites--any one of which this cruise would pay for. Widows do strange things and this choice may be one of them, but when I'm old and the children are grown, my needs will be less, (Don't worry, I'm going to sign up for extended care insurance very soon.)and the money I'm spending on this trip will be insignificant. For now, I'm calling it a really good treatment for my mental health. An investment.
February 2, 2005--6 months post-op
246/147.5/125 DOWN 98.5
I went to Ventura for my 6 month p/o checkup with Barbara from Dr. Rabkin's office. My labs were good, but am a little low on potassium. I'll call my PCP tomorrow for recommendations.
It seems that I'm losing very quickly. I think this is happening because I've really limited my carb intake from the beginning. A little warning was issued: Eat more fruit and whole grain carbs. I only eat whole grains, but really haven't eaten a lot of fruit. The trick will be to eat the protein and then the veggies before I hit the brown rice, or whole wheat pasta and bread.
I'm not worried. I know what I have to do and I will. I was so focused on not taking advantage of the honeymoon period with an overindulgence in carbs because I was afraid, so afraid I'd start to regain weight. I'm going to get in 3 servings of fruit a day, maybe a whole whole wheat English muffin with my eggs in the morning. And so on.
I'm still working on my photos. It's so shocking when I look at my dying self the month before surgery. A stroke waiting to happen.

I'm the happy hippie on the left. Once, it would have been, I'm the happy hippo. . . .
NOVEMBER 27, 2005
So much I've done, so much I've seen 2-1/2 years after I began this profile.
I now weigh 126-128. I work out. I can run. I can walk uphill without breathing hard. I can carry 50# bags of potting soil from the car to far back in my back yard. I can carry and dance with my now 4. 9 year old baby.
The guys aren't exactly lining up at my front door, and Brad (as in Pitt) hasn't parked his shoes under my bed, but I'm actually really enjoying being a single woman--except for the parenting part, and that's terribly difficult, even painful at times.
I'm not shy about going to church, or anywhere, anymore. Baking is a pleasure, even if I don't eat much pumpkin pie. ;>)
There aren't enough words to express my gratitude to my surgeon, and to all the brilliant people in science who developed the DS. The ability to eat a wide range of food and have no fear is pure joy.
Eventhough I can't drink very much of it, I've begun to collect fine wine and bought a wine refrigerator. Hehehehe.
My home is no longer a just a refuge, it is available to me in ways it wasn't before. Not only have I taken on a new life, but my garden has as well.
I was a fast loser, so I graze to maintain my weight. I snack on nuts and seeds, always eat protein first, love fruit, struggle with veggies.
I take a prenatal Rx vitamin and Bariatric Advantage calcium citrate with vits K and D, and magnesium. My labs have been great, with one incidence each of low potassium (corrected after one month on an Rx supplement) and one slightly low iron for which I now take
Nu-iron.
I have more muscle than I did at 6 month post-op. We get strong carrying all of those extra, very heavy fat cells wherever we go. Mine quickly developed by working with resistance machines starting 6 weeks post-op.
Oh, my dears, what a God and science given blessing this has been.
Laughter comes more easily. What else is there to say?
FEBRUARY 27, 2006
So, I drove down to Tijuana from La Canada (between Pasadena and Glendale) on the great PS research quest. It was a little less than a 3 hour trip, including the stop for Mexican insurance. Fortunately, the rain didn't start until we were already there.
I took the essentials with me for a mellow trip: freshly ground and brewed coffee (a combination of 1/2 decaf--Trader Joe's Pacifica--and 1/2 Starbuck's Komodo Dragon a "bold, rich blend"), in a great (large) carafe, a bottle of heavy cream, a bag of Splenda, 30 CDs with everyone from Antigone Rising, The Carter Family recordings 1926-1928, Bob Dylan, Bruce Springstein, to Yoyo Ma, and Zydeco. Oh, and also my book, "The Witch of Cologne"--just in case we got stuck somewhere. I wanted to be prepared.
My journey-mate, Mary, was funny, and sarcastic. She and I are bilingual so we were pretty jazzed about returning to the country where we learned Spanish. I'll loan her to you if you need to have fun during your travels.
I met with Dr. Juan Carlos Fuentes--no relation to Carlos Fuentes, great Mexican writer. He was charming, laughed at my joke , answered all of my questions, and looked me in the eyes when we spoke. We discussed pain management--not that I'm a wimp. . . . I'm not familiar with the post-op med he uses, but he assured me it was as effective as morphine.
He said it was difficult to get morphine as it's a controlled substance, and that it's primarily used by anesthesiologists. They don't have a PCA pump, so that's out, but he said the private duty nurse is very responsive. The take home med he prescribes is Percocet. That made me really, may I say REALLY happy, as I've read some posts here about people only getting Tyelenol .
He gave me the name and telephone number of a patient to call for reference. She'd had an LBL with him. We looked at lots of pictures of women with LBLs and BA, BA/BL, and thigh lifts and he found those with bodies like mine. The incisions were all refined. Depending on the patient's need, he uses the LeJeur (lollipop) incision for BL.
I was shown the OR and recovery room--through a glass-windowed door. LBL patients spend the night in the surgi-center. After that, they are discharged to their hotel.
My DD, an RN, will be there for the in-patient night, and then the 2nd night. It will be great to have her take care of the drains. Because I'm a widder woman, she has a real phobia about me dying. She called 3x while I was gone. Mary will come down to cover the next 2 nights.
Mary and I managed to eat at 2 different restaurants in about a 5 hour time period. She's a RnYer, but I don't hold it against her because as soon as she gets her new insurance, she's going for a revision (too much stomal bleeding). The food was great. She had duck in a raspberry sauce at the first one, I, the quail in a tomato and pepper sauce. The second restaurant was seafood: we shared a combi-platter, but it wasn't the usual fried assortment. Red snapper sauteed in garlic butter; calamari in a tomato cheese sauce; a huge prawn in bacon wrap; a breaded prawn (we didn't eat that one); white fish in a tomato sauce with capers, onions, green olives; a lightly breaded, round, delicately seasoned "stick"; and a heavenly fish soup. It was $10. On the house, they gave us two small drinks that were condensed milk based, frothy with sugar, vanilla and cinnamon. Mary took 2 sips of hers, I drank all of mine. What can I say? I fell off the carb wagon. . . .
I'm scheduled for LBL 4/6. Yeah!
Roz
DS 8/4/04
246/128
MARCH 2, 2006
I've just recovered from 4-6 weeks of monsterdom--cookies, sweet pastries, candy. It took 4 days doing fitday.com and seeing my carbs come down from 100 grams to around 25. By day 4, I was beginning to feel stronger in terms of my will power. Then by day 5 and ever since (10 days) I'm fairly well clear of the craving and still continuing w/fitday.
To break the trail to destruction, I stopped eating so many Atkins bars, upped my protein to over 150gr by drinking every "Designer Chocolate" (from Trader Joe's). To make it more palatable, I mixed it with my 1/2 decaf-1/2 regular coffee.
I also mixed Syntrex' "Roadside Lemonade" with CrystaLite lemonade to make that more pleasant.
I also cut out even whole wheat products.
Somehow, increasing my protein, eating it more often, and strictly adhering to no less than 64 oz of liquid a day, I seemed to experience less craving.
I began to lose by day 3, then it was a lub a day. I'd managed to gain 8# I had eaten so much in those 4-6 weeks. Since then I've averaged about a lub a day. THANK YOU DS!!!
You'll probably get plenty of input here. I did after I desperately screamed out for help. I followed the advice I got.
All is now well in my garden.
Roz
246/130--2 more down to go. By Monday I'll drop the next 2 lubs and be back to 128 where I maintained for 14 months.
I've been more preoccupied with pain and seroma than any other aspect of my LBL. It dawned on me, finally--sometimes I'm a little slow----AARP recommends crossword puzzles for brains like mine----that there are other aspects of the LBL to think about:
Such as:
* working out more for increased strength and, therefore, health
* making sure I have enough pillows for when I get home. (ie head to Walmart)
* my obsession with which compression garment is best (long-legged? medium-legged? waist cincher type?) order online, or go to Nordstrom?
* my obsession with, "Will it really work for me? Will it really tighten my pregnancy and obesity caused rectus diastasus" Is it possible to have that pre-preggers flatness like I see in photos of other women?
I NEVER obsessed about complications and pain pre-DS, gall bladder and appendix removal. And I've had NO complications and took all of 3 Lortab after hospital discharge!
I've decided that these obsessions are standing in the way of a completely positive approach. It's a head thing, right? At least for me.
If I do EVERYTHING I'm supposed to, as I did with the DS, I can rely on my trusty, mellow, reliable body. And, I have my DD, RN, to fuss over me post-op (She can handle the drains in the beginning.)
I felt SO much better after I moved into this freedom. Without being in a positive space I REALLY limit my joy and excitement at the upcoming change. I have ALWAYS recovered quickly. I am not superstitious about thinking there will be anything different about this post-op experience. I know my pain will be adequately attended.
Hmm. I think I'll put this in my profile to review in case I slip and revisit the above obsessions.
Roz--Queen of capital letters and sometime Queen of Exclamation Points!
MARCH 31, 2006
I am feeling a tad overwhelmed by the amount of preparation that seems to be necessary to get ready for my convalescence.
I know I didn't do all of this before my WLS. Granted, my DS was done lap and 5 little incisions are nothing compared to an LBL/MR, but jiminy crickets! this is all SO much to worry about.
What if I forget to buy the Bacitracin ointment; or the batteries for my remote (well, that won't happen because at Christmas time the clerk at Radio Shack talked me into buying their huge jumbo packs of every size batteries made); or, or, or. . . .
Really, I am not at all worried about the surgery itself, my survival, or complications. It's all of this other desiderata that's keeping me in a low grade level of anxiety.
I feel like just saying, o' phooey! devil take the hindmost and tally ho!
I mean I have some pretty pressing issues I have to get taken care of around here, such as planting about 60 summer flowering bulbs and bareroot plants in the ground, and arm wrestling my 9 y/o boy into the shower every morning (he'll just have to go dirty when I'm post-op ;-)).
Then there's the air freshener matter. Can't forget to buy cans of that. Traveling with a friend, one must be as genteel as possibile in the world of shared bathrooms.
Having young children I can't just be as narcissistic as I want to be right now. 3 days before the surgery I have to take the 13 y/o to the Museum of Tolerance in Los Angeles as part of his Anne Frank project. This is a 3-4 hour tour. My late husband and I took our older children several years ago. Sometimes it's hard revisiting sites where we went together. This is one of them. Just another example of something that has to be done that I don't want to do. . . .
Vent. . . . .
The Great Lower Body Lift Journey:
HISTORY OF P/O--OVERVIEW:
Almost 4 WEEKS POST-OP: So much to say, and so little coffee to say it with.
Do you think it's diagnostic of something when a single mother actually looks forward to major surgery, general anesthesia, a couple of weeks of pain, and a trip out of the country to a nation where, gasp, there's no malpractice insurance?
Mary, who has now earned the position of best-friend-for-life, was an extraordinary gift to me. The whole time in Mexico (5 nights) was really something of a lark for the two of us. She'd leave me medicated in our suite, watching a DVD (I'd rented 8 from Blockbuster and brought along the kids’ portable DVD player), with one cup of Roadside Lemonade (in my stainless steel Starbucks' coffee mug) and one cup of freshly ground, shade grown French roast coffee (also in a Starbucks’ mug) on the table next to my lounge/bed.
She explored most of the Zona Rio on foot, discovering the Plaza de Zapatos (shoes), and even a tack shop—her brother had sent her on that mission. She also found a lot of great restaurants. Trust a RnY and a Dser to be always on the lookout for good food.
BajaVicki, of psJourneys.com fame, was also a wonderful help even though I wasn't a client. And on my last journey, to remove the stitches, she picked me up at the Amtrak station in San Diego, transported me across the border, took me to the hotel, and then on to the doctor's office, went to breakfast with me, and then took me back to Amtrak station the next day.
Let me write briefly here about our hotel. I can’t say enough good words about it. Although, the Hotel Real del Rio didn’t have coffee makers, after Mary asked once and I also a little later, low and behold, the management sent out and bought us a maker for the suite. At last, we were in a perfect world.
The chief of housekeeping, Alicia, (a woman who’d spent several years working as a hospice manager and whose major in college had been philosophy) stopped by every day to make sure we had enough water, to plump the pillows under my feet, to talk to me about good post-op nutrition—protein, protein, liquid, liquid (her preference for diuretic purposes: agua de pina, agua de papaya). You’d think she’d been eavesdropping on our board. She even brought me a bag of dried “Jamaica” flowers for an herbal tea that’s supposed to be great for recovery. She also “counseled” about good pain management.
The hotel had wheelchairs and a strong young bellman who always smiled as he wheeled me up and down the ramp to and from the elevators, into the restaurant and out to cabs. The Director General of the hotel remembered all of his guests’ names and spoke fluent English, as did the desk clerks. The food was excellent, the room service came at the speed of light, and the headwaiter told me I was beautiful every day.
THE SURGERY: Lower body lift with muscle repair. The procedure took around 5 hours because there was a lot more muscle repair than Dr. Fuentes expected. If it took him longer than planned, then no wonder it always seemed so impossible to be able to do sit-ups--even after 4 years of regular Pilates' training.
The MR tightened the abdominal rectus muscles that become separated from pregnancy and obesity thus allowing the abdominal distension we often see in spite of countless situps. The LBL is what pulls up the excess abdominal skin, and excess skin in the back where it also lifts the butt. The mons is also "restored". The upper thigh area has some pulling up there, too.
DISCOVERY: There actually are body parts I’d forgotten until I looked down past my flat belly. I actually laughed--ouchy--when we were reintroduced post-op. My navel actually looks like a navel again. After the DS, it was more or less a mere caricature of a bellybutton.
RECOVERY: What a breeze! Following doctor’s orders really plays a powerful role. Knowing that too much activity can contribute to a seroma, kept me as immobile as I’ve ever been. There was NO way I could have found myself up walking the way I did after the lap DS. The first day post-op I stayed in bed except to go to the bathroom. The same was true the following 4 days except for wheelchair rides to the restaurant and the one follow-up trip to the plastic surgeon. I’m still spending a lot of my time in my recliner with my feet up to manage any potential swelling.
I needed to take my pain meds every 3 hours, not every 4-6, and I really tried to stay on top of that because the alternative was just too uncomfortable, mainly because of the extensive muscle repair. I had Percodan and Tramodol drops (very fast acting ), then switched to Vicodin 10/500, still using the Tramadol when I needed to speed things up. 3 weeks post-op, the most of the pain is gone and really only bothers me after sitting for awhile, or if I’ve had to get up and down too much, so I’m probably taking a Vicodin a day and one before bed.
MEDICAL HISTORY P/O:
I stayed overnight at the surgicenter and had pretty intense evening after the 5 hour surgery. Pain meds were ordered for every 6 hours, but that wasn't enough and for some reason, I evolved into a really uncomfortable restless leg state that exacerbated the pain. My daughter, an RN, my advocate, accepted the pain order, but told the nurse that I needed something to calm me down, so Ativan was added to my IV cocktail and that put me out for the night.
I was able to stand almost erect from the first day, then after that I had no problem. There was quite a sensation of tightness, but it wasn't painful. Sort of "scarey"a, but not painful.
I relied on my arm muscles to help me from my reclining position (lying on many pillows), to sideways roll, then also lifted myself on up to standing using my thigh muscles. This procedure seemed the least "stressful".
I did not need a walker, nor a toilet riser.
My drains were removed at day 7. I had very little drainage I think because my body fat is at only 18% of my weight.
I wore my binder for 2 weeks (w/drains clipped to it for 1 week), then switched to the black Veronique. After about a week the side zippers began to dig into my sides and I bought a Spanx and after one accident, cut out the entire crotch. I love this garment.
I had and have very little swelling. The incision is beautiful, symmetrical, and in the back, already just a fine line in places. It is pretty low, certainly no more than 3 inches above my tailbone. What a difference a scalpel, needle and thread make when held in the hands of a plastic surgeon. Pure art.
I did something really stupid and ignorant when I put peroxide on the incision, not once but twice, both times following a shower. I thought I had to "dry" it off. Dr. Fuentes managed to not roll his eyes, but the peroxide sort of ate through the scab and a superficial, very superficial, area was "descabbed" and looked a little gross. I wouldn't call it a separation, but by disrupting the scab I slowed the healing in that area and now the incision looks a little wider there.
Apparently, peroxide actually "eats" red blood cells that form the basis of scabs and that's what led to the breakdown of the scab. He said that the foaming we see is that process at work. At least I think that's what he said. I had some weird memory from my childhood of the foaming being the destruction of infection. . . .
I've got pics right after surgery, then at day 10. Well, actually Dr. Fuentes has the photos and I need to ask him to email them to me. When I can actually corner my overworked daughter, I'll have her take current photos.
WHAT I WOULD HAVE DONE DIFFERENTLY:
I wouldn't have bought the Veronique, although I love the way it looks, after a week the side zippers began to dig in. (That's the week when I began the Stage II garment wearing. Had I known about it, I'd have bought the fabulous Ann Michael garment (that I got in TJ) one size larger (medium) and wish I'd washed the makeup off my hands before I tried putting it on the first time so that I could have exchanged it. The good is that the Spanx I bought here last week is great. I did cut out the entire crotch to the seam line because the opening was a joke.
I wish I'd had more Syntrax Roadside Lemonade protein powder, because I ran out. I've found it harder to keep up my protein count because of that.
I'd have asked for something to put me into a deep sleep at time of immediate post-op recovery. Pain med every 6 hours just isn't (wasn't) enough for me. I got restless legs and the pain broke through. My daughter asked them to knock me out with something and they did, so I CAN say they were very responsive. They just a conservative attitude toward heavy drugs.
I WAS given Percodan for 10 day recovery and that really did the trick, along with Tradol (Tramodol) drops that are VERY fast acting to cover the time between taking the Perc and when it kicks in. Opiods don't both me. Actually, I love them. . . . hehehehe
I think I needed a larger table next to my recliner because I had a hard time managing all the accoutrement of life in a lounger: remotes (3), paperwork, calendar and notepad, candle (I indulge in its soothing aroma and flame everyday), coffee and lemonade mug, etc.
HOME AID:
IMHO, unless there is no other choice, a companion is imperative for the first 10 days to 2 weeks. And, frankly, if there are dependent, young children, I'd say a month of help is the safest and least stressful approach to recovery. Had I no choice, 2 weeks might work, but for me, at my age, I really couldn’t have dealt with preparing 3 meals a day, and all of the other childcare needs that go along with having the little darlings around. Careful hugs and kisses are the least of the challenges. There should absolutely be no lifting for a LONG time.
CONCLUSION:
I love the way I look, even w/a somewhat swollen mons, and waistline. I'm happy with the incision, the pain management I received, the companionship I had with Mary, and my Hawaiian Lomi Recliner (with its mechanical leg/foot lift).
So, dear ones, all is well in my garden. I’m loving my convalescence, my meds, the wonderful people from OH who’ve kept in touch with me, and Mary dear, who still comes every morning to make my coffee, the kids’ breakfasts, and then carpools them to school. What can you say about someone like that????
Well, I’m off to the Lomi Lounger, cup of French roast in hand, an early James Lee Burke (“The Lost Get-Back Boogie”), to put my feet up and hopefully grab a nap before the little darlings come pounding through the front door.
Roz
DS 8/4/04
246/127
LBL/MR 4/6/06
At home, 128 lubs: November 2005

Photos
 128 O, What shall I wear today? November 2005 |
 128 The simple pleasures: A great dog and a velvet outfit |
Member Interests:
Click here to see interests of other ObesityHelp members.
Surgeon Info:
Surgeon: John Rabkin, M.D.
I attended two of Dr. Rabkin's seminar-support group meetings. Both were led by Program Director, Barbara Metcalf, RN. Dr. Rabkin explained medical issues, elaborated on the benefit of the DS over the RnY, and clearly discussed the risk vs benefit for the MO. He pointed out that the risk of death is the same as for other surgeries performed on the MO. It's not the surgery, it's being MO, but it's WLS that gets the bad reputation. He does both DS and RnY, but only the RnY when an insurer won't pay for the DS. He has performed an evolving series of weight loss surgeries since the 70s,and has published in peer review journals. He has trained with the best and is now in the forefront. He is completing the longest range study of post-op WLS patients that has been reported. This 10 year study has the potential to help the MO on many levels. The seminars were rich in information; financial details, medical follow-up, risk vs benefit, availability of local housing for immediate post-op recovery, and aftercare information were all carefully explained. The handouts had just about everything a person would need to be informed. The "Post-ops" were inspiring. Pacific Laparoscopy (Dr. Rabkin's office) produces a calendar every year with B&A photos of his patients. I looked through two year's worth and some of the people were at the seminar. Everyone was great about sharing their experiences. I remain in awe of the revelation of who exists behind the mask of obesity. Other than Barbara, I've only spoken by phone with office staff and they were all friendly. One week after my initial consult at the Ventura, CA satellite office, the authorization request was mailed by Dr. Rabkin's staff. Dr. Rabkin offers a unique arrangement with a local hospital for "cash" patients that has agreed to cap all expenses relating to surgery at $75,000. While this sounds like a lot of money, in the event of complications, we all know how very expensive hospital care is so to have a cap is a blessing. So far, I've found nothing negative to report.
Insurer Info:
Blue Cross/CalPers, PPO
I've hired Larry Slade, Esq., to take my case as high as we can go. BC switched horses midstream. The first 2 denials were based on the "experimental" aspect of the DS. Then, with just 6 weeks to go before they announced the DS would be included and was no longer "investigational", the final denial stated I did not meet the medical criteria. Insurance companies prey on those with few resources, who discourage easily. I am neither of these. It gave me a great deal of satisfaction to write a retainer check to Mr. Slade. Having self-paid, we will be pursuing reimbursement. More later. 2/2/05
Current DS Research
Jan 11, 2008
Obesity Surgery, 17, 1421-1430 (2007) Duodenal Switch: long-Term Results Picard Marceau, MD, PhD1;Simon Biron, MD, MSc1; Frederic-Simon Hould, MD1; Stefane. Lebel, MD1; Simon Marceau, MD1; Odette Lescelleur, MD1; Laurent Biertho, MD1; Serge Simard, MSc2 'Department ofSurgery, Laval University, Laval Hospital, Quebec, Canada; 2Biostatistician Laval Hospital Research Center
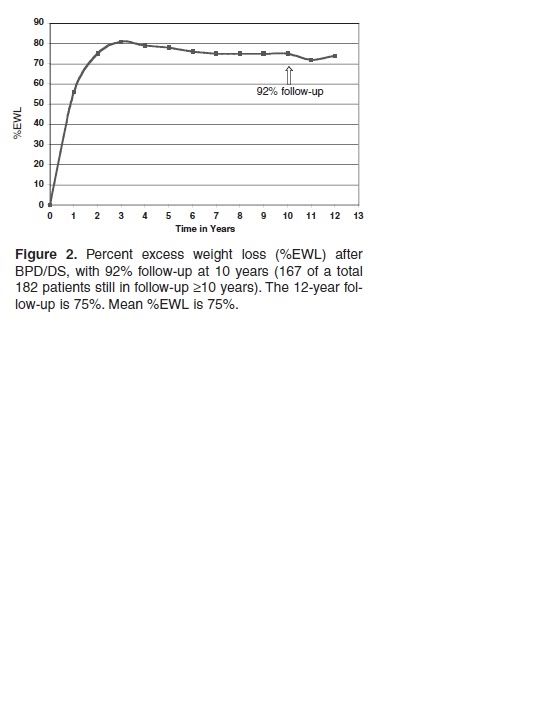
Results: Survival rate was 92% after DS. The risk of death (Excess Hazard Ratio (EHR) was 1.2, almost that of the general population. After a mean of 7.3 years (range 2-15), 92% of patients with an initial BMI > 50 kg/m2 obtained a BMI <35 and 83% of those with an initial BMI >50 obtained a BMI <40. Diabetes was cured (i.e. medication was discontinued) in 92% and medication decreased in the others. The use of the CPAP apparatus was discontinued in 90%, medication for asthma was decreased in 88%, and the prevalence of a cardiac risk index >5 was decreased by 86%. Patients' satisfaction in regard to weight loss was graded 3.6 on a basis of 5, and 95% of patients were satisfied with the overall results. Operative mortality was 1% which is comparable with gastric bypass surgery. The need for revision for malnutrition was rare (0.7%) and total reversal was exceptional (0.2%). Failure to lose >25% of initial excess weight was 1.3%. Revision for failure to lose sufficient weight was needed in only 1.5%. Severe anemia, deficiency in vitamins or bone damage were exceptional, easily treatable, preventable and no permanent damage was documented.
Conclusion: In the long term, DS was very efficient in terms of cure rate for morbid obesity and its comorbidities. In terms of risk/benefit, DS was very sucessful with an appropriate system of follow-up.
****************
Discussion
In our view, morbid obesity is a metabolic disease that extends beyond uncontrolled appetite and abnormal food intake. For the past 25 years, our goal has been to change the basic physiology of these patients, allowing for excess weight loss, maintenance of weight loss and continuation of a normal life. We consider that it is important for quality of life to be able to eat normally. We felt that it was preferable not to concentrate our effort on food restriction, giving a false impression that the only problem is a lack of control of food intake, but rather to target correction of the metabolic dysfunction. In these patients, the difficulty has never been to attain weight loss, but to maintain that weight loss. Morbid obesity should be considered a chronic disease, which requires treatment for life.
The first 8 years (1982-1990), BPD as described by Scopinaro was the procedure of choice within this center. While the results were positive, a decrease in side effects with improvement of absorption were further targets. The procedure was modified successfully. For the last 15 years (1992-2007), DS has been our primary procedure for all patients. This choice has been reinforced with additional knowledge on important involvement of intestinal hormones in the etiology of obesity. It was also reinforced by the high long-term failure rates reported for numerous other procedures.
The present study could be considered exceptional. The Canadian medical system has facilitated an efficient follow-up of a large unselected cohort. We are not aware of any comparable study, using a consistent procedure with such an extended and thorough complete follow-up. Our review shows excellent long-term results after 15 years. Both the weight loss and its maintenance compared favorably with any other procedure. It has the best "cure rate" where cure rate is defined as the absence of morbid obesity: 83% of those with an initial BMI >50 maintained a BMI <40 and 92% of those with an initial BMI <50 maintained a postoperative BMI <35. DS also targeted co-morbidities. It "cured" most diabetic and dyslipidemic patients. For other associated morbidities, results were related to the extent of weight loss, where DS was as efficient as any other procedure.
The reluctance for using DS has been the concern over long-term risks. The present review should be reassuring. The procedure saves lives. A 15-year survival rate of 92% is much better than that of nonoperated morbidly obese subjects and perhaps even better than after RYGBP.8 The operative mortality was found to be comparable to that of RYGBP.13 The long-term risk for malnutrition is real but preventable. Deficiency in albumin, iron, calcium and fat-soluble vitamins requires compliance and medical attention. These deficiencies were rare, they appeared slowly, and were always reversible without permanent damage.
The procedure was relatively secure for bone maintenance. It is possible that with the medical attention provided after surgery, including increased physical activity, better alimentation and appropriate nutritional supplements, the procedure may even be beneficial for bone metabolism, rather than representing a risk.
The negative side-effects with DS were not benign. The unpleasant odor of stool and gas and the frequent abdominal bloating were the price to pay for these patients and it was a major preoccupation for many of them. However, 95% of patients declared themselves satisfied despite this handicap and no one has required reversal of the procedure for this reason. The present evaluation has an important characteristic, in that it is comprised of a non-selected group of patients. No pre-selection was done on the basis of age, BMI, eating behavior, financial or psychological conditions, merits or expected difficulties for follow-up. With appropriate support, the procedure was found to be useful for all groups. Thus, the global applications should be appreciated. We conclude that with a structured and devoted treatment team, DS is a very efficient bariatric operation, to the great satisfaction of both the patients and the care-providers. Finally, one of the striking conclusions of this study is that, in spite of the inherent mortality risk of the bariatric surgery, the long-term outcomes are more positive than the mortality risk without surgery. Furthermore, in spite of the side-effects which are not minimal, the overall patient satisfaction dominates. These two points highlight the profound effect that morbid obesity has, not only on mortality, but also on quality of life.
RnY vs DS Research
Dec 30, 2007
This is a comparison from two papers of the long-term results with the RNY and DS. The RNY study (Shah et al.) can be found at http://jcem.endojournals.org/cgi/content/full/91/11/4223, and the Hess study was published in Obesity Surgery, 15, 408-416 (2004) (I have a .pdf copy if anyone wants to have it).
Even if the curves are oppositely oriented, and one measures percent weight change, and the other percent excess weight lost, and even if you assume that both DSers and RNYers end up at the same initial maximum EWL% (which isn't the case), the curves are pretty directly comparable. The first is from the Shah study; the second is from the Hess study.

FIG. 1. Weight changes among subjects participating in the Swedish Obese Subjects study over a 10-yr period (11 ). There were 627 control subjects who did not undergo bariatric surgery, 156 who underwent banding, 451 who underwent vertical banded gastroplasty, and 34 who had gastric bypass.
Also, there is this study from Christou, reporting long-term RNY results: http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pub med&pubmedid=17060766
in which he reports:
There was a significant increase in failures and decrease in excellent results at 10 years when compared with 5 years. The failure rate when all patients are followed for at least 10 years was 20.4% for morbidly obese patients and 34.9% for super obese patients. CONCLUSIONS: The gastric bypass limb length does not impact long-term weight loss. Significant weight gain occurs continuously in patients after reaching the nadir weight following gastric bypass.
************************
Here are some comments from the bariatric surgeons hired by CHDR (see below) who review appeals of patients who want the DS over the RNY, copied from the California Department of Managed Health Care's decisions: http://tinyurl.com/o4js9
A 60-year-old female enrollee has requested for laparoscopic biliopancreatic diversion with duodenal switch (DS) for treatment of her morbid obesity. Findings: The physician reviewer found that with a BMI of 43.2 and multiple comorbid conditions, the patient met nationally accepted medical necessity criteria for consideration of weight loss surgery. Peer reviewed articles clearly demonstrate superior weight loss and maintenance of weight loss over the long term with the DS as compared to other surgical procedures. Published data also demonstrates that the Roux-en-Y procedure results in as much, if not more, protein calorie malnutrition as the DS. The patient’s assertion that the DS is the most effective surgical weight loss alternative is well supported in the literature and this option was a medically reasonable approach to surgical weight loss. Psychological, nutritional and cardiology evaluations indicated the patient was an appropriate candidate for the surgery.
A 44-year-old female enrollee has requested bariatric surgery including duodenal switch and laparoscopic cholecystectomy for treatment of her morbid obesity. Findings: The physician reviewer found that this patient clearly meets the criteria set by the National Institutes of Health for surgical treatment of obesity. The question raised relates to what would be the best surgical approach. Serious consideration should be given to the medications the patient is likely to take the rest of her life for her SLE and associated joint pain. Specifically, NSAIDs, Methotrexate, Plaquenil, and potential high-dose steroids with exacerbation of SLE symptoms. These medications can predispose the patient to ulcer formation and other gastrointestinal complaints. In comparing the duodenal switch procedure to the standard Roux-en-y gastric bypass, the literature indicates that the duodenal switch has proven to be superior with regard to gastritis, marginal ulcer formation, dumping syndrome, nutritional abnormalities and the stability of the weight loss.
There are many more such statements in the many MANY decisions overturning insurance company denials of the DS on this site. Please have a look.
Regarding CHDR: http://www.maximus.com/corporate/pages/CHDR.asp:
MAXIMUS CHDR is the nation’s leading independent medical reviewer of disputed health insurance claims. CHDR serves more than 25 states in the role of reviewer of appeals made by health plan enrollees. We also are the official Medicare Managed Care Independent Review Entity for the Federal Centers for Medicare & Medicaid Services (CMS). We serve in a similar capacity for the federal Office of Personnel Management (OPM), reviewing claims disputes in connection with the Federal Employee Health Benefits Program (FEHBP).
So you can imagine that Medicare and FEHBP would engage a relatively conservative reviewing agency, to appease their insurance companies -- but their bariatric surgeons believe the DS is best. Go figure.
*****************************
From the Shah paper http://jcem.endojournals.org/cgi/content/full/91/11/4223 (relates primarily to RNY and GB [gastric banding):
| Effect of Bariatric Surgery on Nutritional Status and Intolerance |
|---|
Micronutrient deficiency
Deficiency of iron, vitamin B12, folate, calcium, and vitamin D has been frequently observed after RYGB surgery. Deficiency of vitamin A has also been observed, although less frequently. Nutrient deficiencies after GB surgery are less common because it does not have a malabsorptive component, and an adult multiple vitamin and mineral supplement is considered sufficient to prevent these problems (64). Reviewed below are the studies that have reported nutritional deficiencies in RYGB surgery patients (Table 2![]() ). The majority of these studies were uncontrolled case series, and so it is important to note that the studies may have somewhat overestimated the effect of surgery on nutritional status, especially given that nutritional deficiencies have been noted in severely obese subjects before surgery (65) and that many of the patients are menstruating women who are more likely to have poor iron status.
). The majority of these studies were uncontrolled case series, and so it is important to note that the studies may have somewhat overestimated the effect of surgery on nutritional status, especially given that nutritional deficiencies have been noted in severely obese subjects before surgery (65) and that many of the patients are menstruating women who are more likely to have poor iron status.
|
Serum iron deficiency is seen frequently in RYGB patients (66, 67, 68, 69), with the incidence rate as high as 52% (66). The incidence of anemia (type not specified) has been reported to be as high as 74% (66). Supplements containing usual daily doses of multivitamins (70), and even high doses of oral iron (320 mg twice daily) (71), do not consistently prevent anemia in menstruating women. Contributing factors to iron deficiency anemia include malabsorption due to bypassing of the duodenum and proximal jejunum, the main sites for iron absorption (Fig. 2
|
Vitamin B12 deficiency, assessed by serum vitamin B12 levels, is also frequently seen in RYGB patients (66, 67, 68, 69, 73) with the incidence rate as high as 64% (67). Most vitamin B12 deficiencies in RYGB patients may be corrected by 500 µg/d oral B12 supplementation (74), and a minimum dose of 300 µg crystalline B12 per day is necessary to maintain normal serum levels (75). Only a small number of patients require parenteral administration of B12 (2000 µg/month) (64). Possible factors that contribute to B12 deficiency include achlorhydria (72), which prevents its cleavage from foods; decreased consumption due to intolerance to its main sources (milk and meat) (15); and poor secretion of intrinsic factor needed for its absorption (73). Because of the latter problem, Elliot (64) recommended taking the supplement in a sublingual form.
Serum folate deficiency has been reported to be as high 38% after RYGB surgery (67). Brolin et al. (74) reported that a supplement containing 400 µg of folate per day consistently corrected low folate levels in patients who underwent RYGB surgery, although 1000 µg/d have been recommended by others (64). Primary reason for folate deficiency is decreased folate intake. Malabsorption may not play a big role, even though folate is preferentially absorbed in the proximal part of the small intestine, because absorption can occur along the entire part of the small intestine with adaptation after surgery (76). Maintaining adequate folate levels is important, however, because of the possibility of megaloblastic anemia. Also, there have been reports of neural tube defects in infants born to mothers who underwent RYGB surgery (77, 78).
Calcium and vitamin D deficiency may occur in patients who undergo RYGB surgery, and a deficiency rate of 10% for serum calcium and 51% for serum 25-hydroxy vitamin D levels has been reported (66). PTH levels, however, were not reported (66). Possible contributors to calcium deficiency in the RYGB patients include malabsorption of calcium because of bypassing the duodenum and proximal jejunum in which calcium is mostly absorbed; intolerance to rich sources of calcium such as milk; and defective absorption of vitamin D because of fat malabsorption. Fat malabsorption is due to the short common channel and delayed mixing of fat with pancreatic enzymes and bile salts as a result of bypassing the duodenum. Deficiency of calcium is not always apparent, however, because of release of calcium from bone. Coates et al. (79) and von Mach et al. (80), who followed subjects for 9 and 24 months, respectively, reported elevated markers of bone turnover and/or decreased bone mass in patients who underwent RYGB surgery, compared with patients who underwent GB surgery (80) or the matched obese controls (79, 80). The higher bone turnover in the RYGB patients, however, may be partly due to the increased weight loss in these patients, compared with the other patients. PTH levels were not different between the RYGB and obese control groups (80) nor did they change over time after surgery (79). Nevertheless, to prevent metabolic bone disease, 1200–1500 mg/d of calcium and 400 IU/d of vitamin D supplements are recommended (64, 65). These amounts, however, may not suppress serum PTH or bone resorption, and increased supplementation may need to be considered (81). Because of reduced stomach acid content, calcium citrate rather than calcium carbonate is recommended because the latter requires acid for absorption (64, 65). Regular monitoring of markers of bone resorption such as urinary N-telopeptide level and markers of bone formation such as serum osteocalcin level may also be necessary.
Serum vitamin A deficiency has been reported in 10% of RYGB patients (66, 67). Whereas symptoms of vitamin A deficiency are rare in this population, a case study reported xerophthalmia and nyctalopia in a patient after a duodenal switch gastric bypass surgery due to inadequate vitamin A supplementation (82). A contributing factor to vitamin A deficiency in RYGB patients is fat malabsorption. Careful monitoring of serum vitamin A status and supplementation as needed is necessary to avoid a deficiency.
Despite the evidence of nutritional deficiencies, many surgeons do not recommend adequate supplements or evaluate serum nutrient levels (83), and most patients do not comply with the recommended supplement regimen (70). Education of both the physicians and patients is thus necessary to prevent malnutrition after RYGB surgery.
Macronutrient deficiency and intolerance
Protein deficiency, assessed by serum albumin levels, is less common than most other nutrient deficiencies (Table 2![]() ) (66, 67, 68, 69). To consume enough protein, patients should be advised to consume fish, which is better tolerated than meat.
) (66, 67, 68, 69). To consume enough protein, patients should be advised to consume fish, which is better tolerated than meat.
Simple sugar intake, especially added sugars (64), has been reported to cause dumping syndrome in as many as 76% (84) of the RYGB patients. The food rapidly enters the small intestine causing an osmotic load, which leads to movement of fluid from the blood into the intestine (85, 86). Rapid food entry into the jejunum also stimulates a substantial release of peptide hormones (85, 86). Clinical manifestations of the dumping syndrome include gastrointestinal symptoms such as early satiety, nausea, cramps, and explosive diarrhea and vasomotor symptoms such as sweating, flushing, palpitations, dizziness, and an intense desire to lie down (85). The insulin response is exaggerated and causes hypoglycemia (85, 86). To prevent dumping syndrome, patients should avoid consuming fruit juices and foods and drinks with added sugar (64); consume frequent, small, dry meals because water can make the food more soluble; include dietary fiber; increase dietary protein (especially fish and chicken); and modestly increase dietary fat (to delay gastric emptying) (86).
*************************************
Nobody is trying to make post-ops feel badly about their surgery choice. The DSers postings are aimed at pre-ops and potential revisions, to make sure they know about the DS BEFORE they choose which surgery to have. I'm sorry if that's how our postings make them feel, but that is not our intent.
We DSers also want people to know that we can help people with insurance issues, as most insurance companies can be FORCED to pay for the DS if the patient wants it and is willing to jump through the hoops to appeal -- one of the major independent medical reviewers in the country (used by many insurance companies and the federal government) TOTALLY supports the DS over the RNY when the IMRs are sent to them. Medicare changed their rules in 2006 (in no small part in response to a letter-writing campaign by us DSers!) to include the DS as a covered surgery. As more and more people stand up for their rights to have the surgery of their CHOICE, the insurance companies, one by one, are giving in and making the DS equally available, which is one of our major goals.
About Me
Before & After
rollover to see after photo



