Vertical Sleeve Gastrectomy (VSG) - Also known as Sleeve Gastrectomy, Vertical Gastrectomy
|
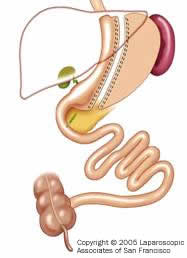
The Vertical Sleeve Gastrectomy procedure (also called Sleeve Gastrectomy, Vertical Gastrectomy, Greater Curvature Gastrectomy, Parietal Gastrectomy, Gastric Reduction, Logitudinal Gastrectomy and even Vertical Gastroplasty) is performed by surgeons worldwide. This forum is titled ?VSG forum? to include the two most common terms for the procedure (vertical and sleeve). The earliest forms of this procedure were conceived of by Dr. Jamieson in Australia (Long Vertical Gastroplasty, Obesity Surgery 1993)- and by Dr. Johnston in England in 1996 (Magenstrasse and Mill operation- Obesity Surgery 2003). Dr Gagner in New York, refined the operation to include gastrectomy(removal of stomach) and offered it to high risk patients in 2001. Several surgeons worldwide have adopted the procedure and have offered it to low BMI and low risk patients as an alternative to laparoscopic banding of the stomach. It generates weight loss by restricting the amount of food (and therefore calories) that can be eaten by removing 85% or more of the stomach without bypassing the intestines or causing any gastrointestinal malabsorption. It is a purely restrictive operation. It is currently indicated as an alternative to the Lap-Band® procedure for low weight individuals and as a safe option for higher weight individuals.
Comparison to prior Gastroplasties (stomach stapling of the 70-80s) 1) Rather than creating a pouch with silastic rings or polypropylene mesh, the VG actually resects or removes the majority of the stomach. The portion of the stomach which is removed is responsible for secreting Ghrelin, which is a hormone that is responsible for appetite and hunger. By removing this portion of the stomach rather than leaving it in-place, the level of Ghrelin is reduced to near zero, actually causing loss of or a reduction in appetite (Obesity Surgery, 15, 1024-1029, 2005). Currently, it is not known if Ghrelin levels increase again after one to two years. Patients do report that some hunger and cravings do slowly return. An excellent study by Dr. Himpens in Belgium(Obesity Surgery 2006) demonstrated that the cravings in a VSG patient 3 years after surgery are much less than in LapBand patients and this probably accounts for the superior weight loss. 2) The removed section of the stomach is actually the portion that ?stretches? the most. The long vertical tube shaped stomach that remains is the portion least likely to expand over time and it creates significant resistance to volumes of food. Remember, resistance is greatest the smaller the diameter and the longer the channel. Not only is appetite reduced, but very small amounts of food generate early and lasting satiety(fullness). 3) Finally, by not having silastic rings or mesh wrapped around the stomach, the problems which are associated with these items are eliminated (infection, obstruction, erosion, and the need for synthetic materials). An additional discussion based on choice of procedures is below. Alternative to a Roux-en-Y Gastric Bypass
First stage of a Duodenal Switch The VSG is a reasonable solution to this problem. It can usually be done laparoscopically even in patients weighing over 500 pounds. The stomach restriction that occurs allows these patients to lose more than 100 pounds. This dramatic weight loss allows significant improvement in health and resolution of associated medical problems such as diabetes and sleep apnea, and therefore effectively ?downstages? a patient to a lower risk group. Once the patients BMI is lower (35-40) they can return to the operating room for the ?second stage? of the procedure, which can either be the Duodenal Switch, Roux?en-Y gastric bypass or even a Lap-Band®. Current, but limited, data for this ?two stage? approach indicate adequate weight loss and fewer complications. Vertical Gastrectomy as an only stage procedure for Low BMI patients(alternative to Lap-Band®and Gastric Bypass) Dr. Johnston in England, 10% of his patients did fail to achieve a BMI below 35 at 5 years and these tended to be the heavier individuals. The same ones we would expect to go through a second stage as noted above. The lower BMI patients had good weight loss (Obesity Surgery 2003). In San Francisco, Dr Lee, Jossart and Cirangle initiated this procedure for high risk and high BMI patients in 2002. The results have been very impressive. In more than 700 patients, there were no deaths, no conversions to open and a leak rate of less than 1%. The two year weight loss results are similar to the Roux en Y Gastric Bypass and the Duodenal Switch (81-86% Excess Weight Loss). Results comparing the first 216 patients are published in Surgical Endoscopy.. Earlier results were also presented at the American College of Surgeons National Meeting at a Plenary Session in October 2004 and can be found here: www.facs.org/education/gs2004/gs33lee.pdf. Dr Himpens and colleagues in Brussels have published 3 year results comparing 40 Lap-Band® patients to 40 Laparoscopic VSG patients. The VSG patients had a superior excess weight loss of 57% compared to 41% for the Lap-Band® group (Obesity Surgery, 16, 1450-1456, 2006). Low BMI individuals who should consider this procedure include:
All surgical weight loss procedures have certain risks, complications and benefits. The ultimate result from weight loss surgery is dependent on the patients risk, how much education they receive from their surgeon, commitment to diet, establishing an exercise routine and the surgeons experience. As Dr. Jamieson summarized in 1993, ?Given good motivation, a good operation technique and good education, patients can achieve weight loss comparable to that from more invasive procedures.? Next: Advantages and Disadvantages of Vertical Sleeve Gastrectomy >> This information has been provided courtesy of Laparoscopic Associates of San Francisco (LAPSF). Please visit the Laparoscopic Associates of San Francisco. |

 email to a friend
email to a friend printer-friendly version
printer-friendly version